|
Academic Year: 2024-2025

|
REPUBLIC OF BENIN
MINISTRY OF HIGHER EDUCATION
AND SCIENTIFIC RESEARCH
UNIVERSITY OF ABOMEY-CALAVI
INSTITUTE OF TRAINING AND
RESEARCH IN COMPUTER
SCIENCE
BP 526 Cotonou Tel: +229 21 14 19 88
http://www.ifri-uac.net Courriel :
contact@ifri.uac.bj
|
|
THESIS
for obtaining a
Bachelor's Degree in Computer Science
Option:
Internet and Multimedia
Presented by :
Adéfêmi Marie-Adelphe AGUESSY
Immersive training in cardiology:
focus on coronary obstructions surgery process with Virtual
Reality
Under the supervision of :
Engineer Lémec AHOUANDJINOU
Examination committee :
|
Maurice COMLAN
|
PhD (Associate Professor)
|
UAC
|
Chair
|
|
Linuse TIKPON
|
Engineer
|
UAC
|
Examiner
|
|
Lémec AHOUANDJINOU
|
Engineer
|
UAC
|
Rapporteur
|
i
Summary
Dedication ii
Acknowledgements iii
Résumé iv
Abstract iv
List of Figures vi
List of Tables vii
List of Acronyms viii
Glossary ix
Introduction 2
1 State of Art 4
2 Conception and technical choices 18
3 Presentation of the solution and discussions 26
Conclusion 33
Bibliography 34
Webography 35
Contents 39
Dedication
ii
To
My father, Adéchokpè Philippe AGUESSY My mother,
Gisèle METONWANOU
iii
Acknowledgements
We express our sincere gratitude to all those who, directly or
indirectly, contributed to the completion of this work:
· God, our Creator, the Most Merciful, for granting us
the health, strength, inspiration, and perseverance needed throughout this
journey;
· Professor Eugène C. EZIN, Director of the
Institute for Training and Research in Computer Science (IFRI), for his
insightful advice and invaluable guidance throughout our undergraduate
studies;
· Professor Gaston G. EDAH, Deputy Director of IFRI, for
his continuous support during these three years of training;
· Our supervisor, Engineer Lémec AHOUANDJINOU,
for his availability, rigor, and willingness to share his knowledge throughout
the development of this project;
· Dr. Burçin ÜNAL, Head of Communication
& Design Department at Alanya University, for her kind support and guidance
during our exchange semester in Alanya;
· Dr Hugues DOGOU, Cardiologist at the Departmental
University Hospital Center of Parakou, for his medical expertise;
· My younger brother, Déo-Gratias, for his
constant and invaluable support;
· My seniors, Nicos HOUNVIO and Lazare FAGBOHOUN, for
their emotional and technical support throughout our undergraduate studies;
· Mr. Parisius Dorian HOUESSOU, Dr. Gervais AFFOGNON,
Dr. Adelphe ADAMBADJI and Mrs Eugenie HOUNGBO for their insightful technical
advice and unwavering support;
· The administration and entire teaching staff of IFRI,
for the quality of the training provided and their professional guidance;
· All the staff of IFRI, for their dedication to
providing a conducive environment for learning and academic success;
· My family, friends, and all those who contributed
through their support, encouragement, and inspiration to the success of this
work;
· Finally, to all those who, through their daily
commitment, inspire change, kindness, and progress in their communities.
iv
Abstract
Training in interventional cardiology is a major challenge in
preparing medical students and young surgeons in Benin. Virtual reality (VR) is
now emerging as an innovative technology which offers new educational
opportunities in this field. Our study is part of this dynamic and proposes the
design and development of an immersive VR software, called CardioTrain,
dedicated to the simulation of coronary revascularisation procedures, in
particular coronary angioplasty (PCI) and coronary artery bypass grafting
(CABG). The software allows users to navigate a virtual operating theatre,
manipulate surgical instruments and follow either a guided course or an
autonomous mode. This approach promotes the gradual acquisition of technical
skills, familiarisation with surgical equipment and a better understanding of
the mechanisms involved in coronary obstructions. The solution was developed
using tools such as Blender for 3D modelling, Unity for interactive
implementation, and a customised SDK for VR integration. Tests confirmed the
prototype's viability. Through this work, we believe we are making an
innovative contribution to medical training in Benin by setting up an
accessible, immersive and scalable tool that could ultimately enrich teaching
practices and improve the quality of learning in interventional cardiology.
Key words: virtual reality, interventional
cardiology, angioplasty, coronary artery bypass grafting, medical training.
Résumé
La formation en cardiologie interventionnelle
représente un enjeu majeur pour la préparation des
étudiants en médecine et des jeunes chirurgiens au Bénin.
La réalité virtuelle (RV) s'impose au-jourd'hui comme une
technologie innovante offrant de nouvelles perspectives pédagogiques
dans ce domaine. Notre étude s'inscrit dans cette dynamique et propose
la conception et le développement d'une application immersive en RV,
nommée CardioTrain, dédiée à la simulation des
interventions de revascularisation coronarienne, notamment l'angioplastie
coronaire (PCI) et le pontage aorto-coronarien (CABG). L'application permet
à l'utilisateur d'évoluer dans un bloc opératoire virtuel,
de manipuler des instruments chirurgicaux et de suivre soit un parcours
guidé, soit un mode autonome. Cette approche favorise l'acquisition
progressive des compétences techniques, la familiarisation avec le
matériel opératoire et une meilleure compréhension des
mécanismes liés aux obstructions coronaires. Le
développement de la solution s'est appuyé sur des outils tels que
Blender pour la modélisation 3D, Unity pour l'implémentation
interactive et un SDK adapté pour l'intégration VR. Les tests
réalisés ont confirmé la viabilité du prototype.
À travers ce travail, nous estimons apporter une contribution innovante
dans le domaine de la formation médicale au Bénin, en proposant
un outil accessible, immersif et évolutif, qui pourrait à terme
enrichir la pratique pédagogique et améliorer la qualité
de l'apprentissage en cardiologie interventionnelle.
Mots clés : réalité
virtuelle, cardiologie interventionnelle, angioplastie, pontage
aorto-coronarien, formation médicale.
vi
List of Figures
1.1
|
Coronary arteries
|
5
|
1.2
|
Touch Surgery (by Medtronic)
|
10
|
1.3
|
WebSurg home interface
|
10
|
1.4
|
Surgery Squad home interface
|
11
|
1.5
|
VCSim3 complete set-up including the simulator software
running on the laptop, VSP haptic device, fluoroscopic view console, balloon
inflation device, and contrast injec-
|
|
|
tion syringe
|
14
|
1.6
|
Screen captures from the virtual reality-extracorporeal
circulation (VR-ECC) simulator, featuring from left-to-right: adjustment of the
venous occluder (A), removal of the a clamp from the arterial line (B), an
overview of the heart-lung machine (C), and the
|
|
|
menu system by which users navigate through the simulation (D).
|
15
|
1.7
|
home page of the official vCathlab website
|
15
|
1.8
|
Image courtesy of Osso VR.
16
|
|
2.1
|
Use case diagram
|
19
|
2.2
|
Sequence diagram for the use case "Simulate surgery on an
obstructed heart"
|
20
|
2.3
|
Operating room design in Blender
|
22
|
2.4
|
Using the Unity3D engine to create the VR experience
|
22
|
2.5
|
Script for animating the user's hands written in Visual Studio
2017
|
23
|
2.6
|
Adobe Illustrator interface screenshot
|
24
|
3.1
|
CardioTrain Logo
|
26
|
3.2
|
CardioTrain Color Palette
|
27
|
3.3
|
CardioTrain logo variations
|
28
|
3.4
|
A few examples of the logo in use
|
28
|
3.5
|
Home interface
|
29
|
3.6
|
Selecting and choosing an instrument
|
29
|
3.7
|
Assisted CABG
|
30
|
3.8
|
some 3D operating room exploration screenshots
|
30
|
3.9
|
some 3D hearts exploration screenshots
|
31
|
|
List of Tables
vii
1.1 Comparison of VR Solutions for Cardiology Training 16
viii
List of Acronyms
AR :
Augmented Reality 11, 22, 23,
CABG :
Coronary Artery Bypass Grafting 7, 9, 18, 32,
CAD:
Coronary Artery Disease 4-6,
CardioTrain :
A platform that supports practical training in the treatment
of coronary obstructions iv, 26-28,
CVDs :
Cardiovascular diseases 4,
MR :
Mixed Reality 11,
NSTEMI :
Non-ST-Elevation Myocardial Infarction 6,
PCI :
Percutaneous Coronary Intervention 6, 7, 18, 32,
STEMI:
ST-Elevation Myocardial Infarction 6,
UML :
Unified Modeling Language 19,
VR :
Virtual Reality iv, vii, 4, 12-17, 19, 20, 22-25, 32, 39,
ix
Glossary
AR : Immersive technology which overlays digital content onto
the
real-world environment. viii
CABG : also known as coronary bypass surgery, it's a surgical
procedure
that restores normal blood flow to the heart by creating new
pathways around narrowed or blocked coronary arteries. viii
CAD: common type of heart disease which affects the main
blood ves-
sels that supply blood to the heart, called the coronary
arteries. viii
CardioTrain : This is the name of our
virtual reality software that supports practical training in the treatment of
coronary obstructions. viii
CVDs : are a group of disorders of the heart and blood
vessels and in-
clude coronary heart disease, cerebrovascular disease,
rheumatic heart disease and other conditions. viii
MR : Immersive technology which combines
real and virtual environ-
ments with real-time interaction between physical and digital
objects.. viii
NSTEMI : It's a type of heart attack where a
coronary artery is partially
blocked, reducing but not completely cutting off the blood
supply to part of the heart muscle. viii
STEMI: It's a severe type of heart attack where a major
coronary artery
is completely blocked, cutting off blood supply to a
significant portion of the heart muscle. viii
UML : It is a pictogram-based graphical modelling language
designed
as a standardised method of visualisation in the fields of
software development and object-oriented design. viii
Glossary Glossary
1
VR : Immersive technology with a fully immersive
environments where users are completely cut off from the physical world.
viii
2
General introduction
Cardiovascular diseases (CVDs) are the leading cause of death
globally, taking an estimated 17.9 million lives each year [10], particularly
in developing countries. Among them, coronary artery disease, caused by
coronary artery obstruction, represents a critical pathology that requires
rapid and precise management. While cardiology education in medical training
programs, including in Benin, provides students with solid knowledge, their
first hands-on interventions often occur directly on human patients, a
situation likely to generate stress and uncertainty during initial clinical
procedures. To mitigate these challenges and provide a safer, more controlled
learning environment, immersive technologies such as virtual reality have
emerged as a promising solution. By recreating complex clinical environments in
a safe, interactive, and reproducible way, virtual reality offers an ideal
framework for progressive skill acquisition. This is the background to our
project: to develop a virtual reality training tool dedicated to the
acquisition of skills linked to the treatment of coronary obstructions.
Problem statement
The progressive acquisition of initial practical skills in
cardiology, including in contexts such as Benin, represents a key stage before
students perform their first real interventions on patients. In this context,
immersive technologies offer promising opportunities to enrich this stage,
which raises the following central question: how can an immersive virtual
reality application be designed to effectively support the progressive
development of cardiology students' practical competencies, particularly in the
treatment of coronary artery disease?
Objectives
The general objective of this thesis is to develop an
immersive virtual reality application designed to train healthcare
professionals in the management of cardiovascular diseases, in particular
coronary artery obstructions. The specific objectives of this thesis are:
· Provide an interactive environment for learning cardiac
anatomy and medical procedures;
· Reinforce clinical skills through simulations based on
real cases;
· Support medical decision-making between procedures such
as coronary artery bypass grafting
Glossary Glossary
3
and revascularisation;
· Design a scalable software architecture that will
enable the application to be extended to other medical specialities.
Methodology (briefly)
The methodology adopted combines theoretical research into
cardiovascular disease and immersive technologies, with agile development of
the application. It comprises the following stages:
· Documentary analysis and collection of pedagogical
needs;
· Design of models and 3D modelling of anatomical
elements;
· Integration into a virtual reality engine (Unity);
· Programming of interactions and clinical scenarios;
· Testing and adjustments
Structure of the document
This thesis is structured around three main chapters.
The first chapter lays the theoretical foundations for our
study. It presents the medical context of coronary artery disease and the
issues involved in training cardiology students to manage it. It also provides
a critical analysis of existing solutions, highlighting their advantages and
limitations.
The second chapter is devoted to the design of the system
developed. It describes the technical choices made and uses UML modeling to
illustrate the main interactions through use case and sequence diagrams. The
use of tools such as Unity and Blender is also justified, in view of the
project's educational and immersive objectives.
Finally, the third chapter outlines the results obtained from
implementing the system, while highlighting the difficulties encountered. It
concludes with an outlook on possible improvements and future developments for
the project.
4
Chapter1
State of Art
Introduction
In order to lay the theoretical and scientific foundations
for our work, it is essential to examine the research and solutions already
developed in similar fields. This chapter takes this approach by proposing an
in-depth analysis of what already exists, with the aim of placing our project
in its academic, medical and technological context. We begin by presenting the
key concepts relating to cardiovascular disease, with particular emphasis on
coronary artery disease, and the issues involved in training cardiology
students. We will then explore the contribution of immersive technologies, in
particular virtual reality, to medical learning. Particular attention will be
paid to existing applications of VR in cardiology, in order to identify
advances, shortcomings and future prospects. This review will identify the
foundations on which our approach is based, while justifying the relevance of
the proposed solution to improving specialized medical training.
1.1 Coronary artery diseases
1.1.1 Overview
Cardiovascular diseases (CVDs) are a group of troubles
affecting the heart and blood vessels. They include conditions such as coronary
heart disease, cerebrovascular disease, rheumatic heart disease, and others
[10].
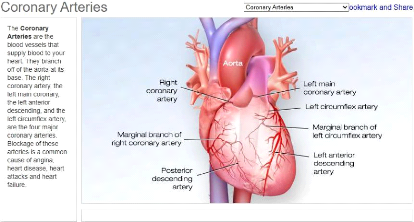
Among these, coronary artery disease (CAD) is one of the most
common and serious forms, and remains a major cause of morbidity and mortality
worldwide. Coronary artery disease occurs when the coronary arteries, which
supply oxygen-rich blood to the heart muscle, become narrowed or blocked. This
is typically the result of atherosclerosis, a process characterized by the
accumulation of fatty deposits (plaques) on the inner walls of the arteries.
Over time, these plaques harden and restrict blood flow to
the heart. If a plaque ruptures, it can cause a blood clot, leading to a heart
attack [9].
[9] The development of CAD is influenced by modifiable
lifestyle factors such as smoking, exces-
Chapter 1. State of Art 1.1. Coronary artery diseases
Figure 1.1: Coronary arteries
5
sive alcohol intake, poor diet, physical inactivity, and
chronic stress, as well as medical conditions including type 2 diabetes,
hypertension, and chronic kidney disease. Genetics and aging also contribute,
highlighting the importance of prevention and early detection.
Symptoms of CAD often appear gradually and can be subtle.
Typical signs include angina (chest pressure or pain), shortness of breath,
fatigue, dizziness, cold sweats, or nausea. Symptom presentation can vary by
sex, with men often exhibiting classic chest pain, while women may experience
atypical signs such as back or jaw discomfort, sleep disturbances, or anxiety.
This variability underscores the need for advanced training tools capable of
simulating diverse clinical scenarios to improve diagnosis and treatment
skills.
1.1.2 Coronary artery disease's treatments
Treatment of coronary artery disease (CAD) aims to relieve
symptoms, slow or reverse disease progression, and reduce the risk of heart
attacks and death. The therapeutic approach often depends on the severity of
the blockage, the presence of symptoms, and the overall health status of the
patient.
· Lifestyle and medical management:
In early or moderate stages, CAD may be managed through
non-invasive methods, including:
- Lifestyle modifications: Patients are
advised to stop smoking, reduce alcohol intake, adopt a healthy diet (e.g., low
in saturated fats and sodium), exercise regularly, and try to manage stress.
- Pharmacological treatments: they include
statins to lower cholesterol, beta-blockers to reduce heart rate and blood
pressure, antiplatelet agents such as aspirin to prevent clot formation, ACE
inhibitors and calcium channel blockers for blood pressure control, among
others.
These treatments are usually the first line of defense and may
significantly improve quality of life and prognosis.
· Chapter 1. State of Art 1.1. Coronary artery
diseases
6
Interventional procedures
When medical treatment is insufficient or significant
arterial blockage is present, more invasive procedures may be necessary. The
choice of procedure depends on the individual case and its severity, aiming to
achieve the best possible patient outcome.The most common procedures
include:
- Percutaneous Coronary Intervention
(PCI)
Also known as angioplasty, Percutaneous
Coronary Intervention (PCI) is a minimally invasive procedure to restore blood
flow in arteries narrowed or blocked by atherosclerotic plaque. During the
procedure, a flexible catheter is carefully inserted through the groin or wrist
and guided to the heart. Once at the blockage, a small balloon is inflated to
widen the artery, and in most cases, a stent is then placed to keep the artery
open.
PCI is a cornerstone of modern cardiology, indicated in acute
cases like STEMI as an emergency reperfusion strategy, in high-risk NSTEMI or
unstable angina patients, and in chronic CAD when symptoms persist despite
optimal medical therapy or when significant multi-vessel or left main disease
is present.
Instruments and medical equipment used
The setup for PCI requires specialized lab infrastructure and a
comprehensive arsenal of
instruments to safely treat coronary artery disease. We can
mention [18]:
* Operating table;
* Catheters (guide catheters, balloon catheters and aspiration
catheters);
* Stents ;
* Contrast dye;
* Guidewires ;
* Fluoroscopy and imaging equipment called angiography suite ( a
C-arm X-ray ma-
chine or biplane imaging system, digital monitors for live
image display, radiation
protection systems and integrated control consoles for the
interventional team);
* Pressure transducers and hemodynamic monitors;
* Sheaths and introducers;
* Cardiac defibrillator and emergency resuscitation
equipment;
* Patient monitoring system (ECG, pulse oximeter, etc.) ;
Risks, complications, and how they are
managed
Although Percutaneous Coronary Intervention (PCI) is generally
safe and routine, it carries some risks typical of invasive procedures. Most
complications are rare, but awareness is crucial for clinical practice and
understanding patient outcomes. Common risks include: * Bleeding or
hematoma at the catheter insertion site, especially with femoral
access. That's why careful post-procedure monitoring is essential. Manual
compression or vascular closure devices are often used to prevent
complications.
* Allergic reactions to the contrast dye can
occur, particularly in patients with a history of allergies or kidney issues.
In such cases, premedication or low-osmolar contrast agents are usually
recommended.
Chapter 1. State of Art 1.1. Coronary artery diseases
7
* Vascular injuries, like arterial dissection
or perforation, are rare but serious. These may require immediate endovascular
repair or, in extreme cases, emergency surgery.
* Arrhythmias (irregular heartbeats) might
happen during the procedure when instruments pass through the coronary
arteries. Most of the time, they're brief and managed with medications or
temporary pacing if needed.
* There's also a chance of restenosis
(artery narrowing again) or heart attack, but the use of drug-eluting
stents and dual antiplatelet therapy (DAPT) has significantly reduced this risk
over time.
In real-life practice, managing complications depends on a
skilled medical team, close monitoring, and good planning before the procedure.
Overall, the benefits of PCI clearly outweigh the risks ,especially for
patients with severe angina or acute heart attacks.
- Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting (CABG) is a major heart
surgery with the same aim as the PCI defined above: to treat coronary
obstructions.
However,its technique is special: to «bypass» the
blocked arteries. Surgeons take a healthy blood vessel,often from the patient's
leg (saphenous vein) or chest (mammary artery) and graft it onto the heart to
reroute blood flow around the blockage. It's like building a new road when the
highway is closed.
CABG becomes necessary when medications and lifestyle changes
aren't enough or angioplasty (with stents) isn't a good option or the blockages
are too many or too complex.
Patients who benefit most from CABG usually have multiple
blocked arteries or diabetes or reduced heart function (especially in the left
ventricle).
Instruments and medical equipment used
Coronary Artery Bypass Grafting (CABG) relies on specialized
instruments and machines that support every stage of the complex surgery, from
opening the chest to maintaining circulation and performing precise vessel
grafting. [20]
* Operation table, pressure transducers, hemodynamic monitors
and patient monitoring system (ECG, Pulse oximeter, etc.) as for PCI ;
* Heart-Lung machine (Cardiopulmonary Bypass Machine);
* Dissection instruments ( scissors, forceps, scalpels, sternal
saws, and dissectors);
* Cannulae (arterial and venous tubes);
* Vascular grafts;
* Surgical retractors;
* Surgical sutures and needle holders; * Electrocautery
devices;
* Perfusion systems;
* Suction devices;
* Aortic punch and clamp [21] ;
Chapter 1. State of Art 1.2. Cardiology training issues
8
Risks, complications, and how they are
managed [23]
Even though Coronary Artery Bypass Grafting is a common and
life-saving surgery, it's important to understand that it comes with its share
of risks and possible complications. Some of the main risks include infections
at the incision site, bleeding during or after surgery, and issues related to
anesthesia. There's also a risk of irregular heart rhythms, like atrial
fibrillation, which can happen after surgery and may require medication or
further treatment.
More serious but less common complications can involve
stroke, heart attack, kidney problems, or lung issues. The surgical team is
always prepared to monitor for these and manage them quickly. For example,
antibiotics are given to prevent infection, and blood thinners may be used to
reduce the risk of clots.
Doctors also closely watch the patient's vital signs and use
advanced monitoring to catch any problems early. The recovery period includes
careful follow-up to ensure the heart is healing well and the new grafts remain
open.
1.2 Cardiology training issues
1.2.1 Current methods of training cardiology students
with contextual focus on Benin
In Benin, most of the cardiology education for future
specialists begins at the large Faculty of Health Sciences ( FSS ) of the
University of Abomey Calavi (UAC).
The FSS offers the degree called "Diplôme d'Études
Spécialisées des Maladies du Coeur et des Vaisseaux"[44, 45],
which includes theoretical lectures, classroom case studies, and occasional
practical exposure in affiliated hospitals such as Cotonou's National
University Hospital Hubert Koutoukou Maga.
Clinical rotations are mostly done at teaching hospitals like
the cardiology unit of the University Hospital in Cotonou, where students
observe procedures like ECGs, diagnostic angiographies, or rounds in
consultation and emergency services.[24] Unfortunately, due to limited
infrastructure and a high patient to student ratio, hands-on opportunities are
rare. The learning remains largely observation-based, with medical interns and
residents performing most interventions. According to some of those
students,theoretical knowledge is reinforced through seminars, lectures, and
case discussions led by senior cardiologists. However, advanced simulation
tools or structured procedural training labs are largely absent. The reliance
on traditional pedagogy reflects broader resource constraints in the health
sector and highlights a gap between classroom learning and actual clinical
competence. And in the end, their first real experience still happens directly
on a human patient.
1.2.2 Limitations of the theoretical approach
alone
In medical training,especially in cardiology,theoretical
knowledge is indispensable. However, it has a critical flaw: it prepares
students to know, but not necessarily to do.
In Benin, as in many countries with limited access to simulation
technologies,the only option left is to «learn on the
job», with all the risks that entails. Then, students often move
directly from theory to real-life practice... on real patients.
This situation raises both educational and ethical
concerns.
Chapter 1. State of Art 1.2. Cardiology training issues
9
A student might learn, in theory, how to manage a myocardial
infarction or perform an angioplasty, but their first real attempt often takes
place on an actual patient. There is no buffer, no rehearsal stage. Classrooms
teach equations and diagrams but not stress, uncertainty, or the weight of
holding a catheter when someone's life is at stake.
The result?
· Students feel unprepared and insecure, especially in
high-stakes procedures like those found in interventional cardiology.
· Patients, often unaware, become the first practice
ground, exposing them to potential risks.
· Instructors struggle to bridge the gap between
abstract knowledge and real-time performance under pressure for their
students.
This theory-practice gap is not a new problem. It has been
widely documented in international research. A study published in BMC Medical
Education (2020) highlights that students without early exposure to
simulation-based practice experience higher anxiety levels and reduced
performance in clinical situations. [25, 26]
1.2.3 Complication and error rates in initial coronary
surgery experiences
Several studies have documented measurable differences in
operative performance and complication rates during a surgeon's first
procedures, particularly in coronary artery bypass grafting (CABG).A
retrospective study conducted between 2008 and 2014 analyzed 1,668 CABG cases
performed by 21 surgical residents, each of whom had performed between 32 and
101 procedures under supervision. In their first 30 cases, residents
demonstrated a significantly longer operative time, an average of 29.7
minutes longer than experienced surgeons. This delay was
attributed primarily to longer incision-to-bypass
times (+13 minutes) and extended closure durations.
Importantly, these extended operative times did not correspond with higher
30-day mortality rates or major postoperative complications. [27].
In a separate analysis using data from the Society of
Thoracic Surgeons (STS) Adult Cardiac Surgery Database, 1,195 robotic-assisted
CABG procedures were evaluated across 114 surgeons with no prior experience in
robotic techniques. The first 10 cases for each surgeon revealed:
· A conversion rate drop from 7.7% to 2.5%,
· A major morbidity or mortality rate decline from 21.7% to
12.9%,
· A procedural success increase from 72.9% to 85.3% [28]
These findings confirm that the initial learning curve in
coronary surgery is associated with quantifiable performance differences,
particularly during the earliest procedures, despite adequate supervision and
safety measures.
1.2.4 Existing digital solutions (Excluding immersive
technologies)
Various non-immersive digital tools, including mobile apps,
web platforms, and simulation software, are used to train healthcare
professionals in cardiology, enhancing knowledge and clinical decision-making
skills.
· Chapter 1. State of Art 1.2. Cardiology training
issues
10
Touch Surgery (by Medtronic):
Touch Surgery is a mobile surgical simulation app used
globally to teach step-by-step procedures in various specialties, including
cardiovascular surgery. It offers interactive, gamified modules that guide
learners through virtual procedures using touchscreen gestures and 3D
animations.

Figure 1.2: Touch Surgery (by Medtronic)
· WebSurg :
WebSurg is a free online surgical training platform developed
by the IRCAD (Research Institute against Digestive Cancer). It provides a
comprehensive library of educational resources, including high-definition
surgical videos, expert commentaries, clinical case discussions, and
theoretical modules covering over 100 surgical procedures and specialties.It
supports multiple languages and is accessible worldwide, making it a valuable
tool, especially for professionals in regions with limited access to in-person
surgical training.
Figure 1.3: WebSurg home interface
· Surgery Squad:
Surgery Squad is an interactive web-based platform that
allows users to virtually perform various surgical procedures, such as coronary
bypass, appendectomies, and knee replacements, through guided, step-by-step
simulations. Designed primarily for educational outreach and
Chapter 1. State of Art 1.3. Immersive technologies in the
medical field
11
public engagement, it simplifies complex surgical processes and
makes them accessible to non-experts.
Figure 1.4: Surgery Squad home interface
1.3 Immersive technologies in the medical
field
Immersive technologies refer to digital systems designed to
simulate reality or extend it, allowing users to experience environments that
feel engaging, realistic, or entirely fabricated. These technologies create a
sense of «being there», often through multisensory input,visual,
auditory, and sometimes tactile making users feel mentally and physically
involved in the experience. Their core objective is to blur the line between
the physical and the digital world.[2] Several forms of immersive technologies
exist, each with specific characteristics and applications:
· Virtual Reality (VR): Fully immersive environments
where users are completely cut off from the physical world.
· Augmented Reality (AR): Overlays digital content onto
the real-world environment.
· Mixed Reality (MR): Combines real and virtual
environments with real-time interaction between physical and digital
objects.
Each of these technologies has made significant advances in
education, design, health, and entertainment. However, not all are equally
mature or widely implemented.
1.3.1 Virtual Reality as a key immersive technology in
medical training
While AR and MR are promising, Virtual Reality stands out
today as the most established and widely adopted immersive tool in medical
training. Its ability to simulate real-world procedures in a safe and
controlled environment without risk to patients has made it a go-to modality
for teaching anatomy, surgery, and complex decision-making. Its effectiveness
relies on three core pillars: presence (feeling «there» in the
virtual world), immersion (full sensory engagement), and interaction
(manipulating
Chapter 1. State of Art 1.3. Immersive technologies in the
medical field
12
virtual objects with immediate feedback), which together
transform passive learners into active participants, enhancing procedural
memory and reflex development.[30]
In addition, recent hardware improvements and decreasing
costs have made virtual reality more accessible to universities, hospitals, and
simulation centers around the world.
1.3.1.1 Types of Virtual Reality experiences in medical
education
All VR systems are not created equal. In medical education,
they are typically categorized into three main types, depending on their level
of immersion and technological complexity:
· Non-Immersive VR which is desktop-based, and allows
users to interact with 3D environments via a screen, keyboard, and mouse
without full sensory immersion. Despite its limitations, it enables students to
explore anatomy and simulate basic procedures.
· Semi-Immersive VR which uses large screens,
projectors, or CAVE systems to provide partial immersion. It enhances spatial
perception compared to non-immersive VR while still allowing real-world
interaction. These setups are ideal for group training or large-scale
visualizations.
· Fully Immersive VR which places users entirely inside
a virtual environment using head-mounted displays (HMDs), motion tracking, and
sometimes haptic feedback. Users' movements are mirrored in the simulation,
allowing precise surgical gestures and emergency responses.
1.3.1.2 Tools and equipment in VR training
To ensure effective medical training through VR, a
combination of specialized hardware and software is essential. These tools work
together to replicate real-life medical scenarios as closely as possible:
· Head-Mounted Displays (HMDs)
These wearable devices display the virtual environment and
track the user's head movements. Common models include Meta Quest 2 / Quest 3 ,
HTC Vive Pro and Pico Neo 3 / 4 .
· Motion controllers and hand tracking
Controllers enable interaction with virtual tools, such as
scalpels or syringes. More advanced systems support hand tracking, allowing the
user's hands to be visualized and used directly in the simulation. They are
useful in suturing, palpation, or tool manipulation.
· Haptic feedback devices
These simulate tactile sensations like pressure, vibration,
or resistance. Haptic gloves or instrument handles can recreate the feeling of
cutting tissue, inserting needles, or stitching skin. Example: HaptiTouch or
ImmersiveTouch provide physical feedback during simulated surgery.
1.3.1.3 Modalities of use in medical
education
VR is transforming multiple facets of medical education,
providing experiential learning in a controlled, repeatable, and safe
environment. Below are key application areas:
· Skills training: VR allows repeated practice of
clinical techniques such as incision making, endoscopy, cardiopulmonary
resuscitation (CPR) or suturing without using real patients or cadavers.
·
Chapter 1. State of Art 1.4. VR applications in cardiology
13
Surgical simulation: Step-by-step rehearsal of complex procedures
like laparoscopy, arthroscopy, or spinal fusion. Users receive feedback on
precision, speed, and safety.It's used by residents to supplement operating
room training.
· Anatomy education: 3D exploration of body systems with
the ability to rotate, dissect, or zoom into structures in ways that static
atlases cannot offer.
· Clinical decision-making: Virtual patients with
diverse symptoms can be examined, diagnosed, and treated in real-time. This
helps students practice diagnostic reasoning, triage, and treatment
planning.
· Empathy and communication training: Some VR
experiences place learners in the shoes of patients such as those with
dementia, vision loss, or chronic pain to foster empathy and improve
communication.
· Patient education: VR is also used to help patients
understand their upcoming procedures, reducing anxiety and improving
compliance.
· Case study: Stanford's Immersive Learning Initiative
integrated VR surgical training into its curriculum and reported that learners
demonstrated: [31]
- Increased procedural confidence
- Improved knowledge retention
- More accurate performance under pressure
1.3.2 Pedagogical benefits and cognitive impacts of
immersive technologies
Immersive technologies, especially VR, enhance medical
education by transforming how learners acquire, retain, and apply knowledge.
This section highlights their contributions through both pedagogical frameworks
and insights from cognitive science, offering controlled, responsive, and
adaptive environments for high-stakes learning.
These technologies enhance engagement and active learning in
line with constructivist learning the-ory[3], improve
retention and knowledge transfer [32], reduce cognitive load while fostering
spatial understanding [33], enable learners to receive immediate feedback and
learn from errors, support social and clinical reasoning through emotional and
empathy training [34], and strengthen self-efficacy and confidence before real
clinical practice [35], among other benefits.
1.4 VR applications in cardiology
1.4.1 Existing projects and tools in cardiology
training
The use of virtual reality in cardiology has gained momentum
in recent years, offering new ways to teach, simulate, and understand complex
cardiac procedures. Several VR-based tools and initiatives are already being
used or developed for training medical professionals in cardiovascular
medicine. Let's talk about some of these immersive solutions.
· Chapter 1. State of Art 1.4. VR applications in
cardiology
14
VCSim3 (Virtual Catheter Simulator)
VCSim3 is a virtual reality simulator designed for
cardiovascular interventions, focusing on the manipulation of catheters and
guidewires. Developed at Erasmus MC, it uses an inextensible Cosserat rod model
to simulate the mechanical behavior of these tools with sub-millimetre
accuracy. This allows trainee cardiologists to practice procedures like stent
deployment and angioplasty in a safe, virtual environment. VCSim3 enhances
surgical training by providing a risk-free alternative to traditional methods,
eliminating ethical concerns and reducing costs associated with patient,
animal, or cadaver use. Although still a prototype, it shows promising
potential for medical training programs.
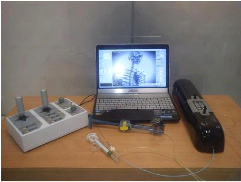
Figure 1.5: VCSim3 complete set-up including the simulator
software running on the laptop, VSP haptic device, fluoroscopic view console,
balloon inflation device, and contrast injection syringe
· VR-ECC Simulator (Extracorporeal Circulation
Training)
The VR-ECC Simulator is an advanced virtual reality training
tool designed specifically for perfusionists. It focuses on enhancing the
skills required for extracorporeal circulation (ECC), a critical procedure used
during cardiac surgeries to temporarily support the heart and lung functions.
Developed with cutting-edge technology, including Unreal Engine 4 and Autodesk
Maya, this simulator offers an immersive and interactive experience. It allows
healthcare professionals to practice and refine their techniques in a safe,
controlled virtual environment. The VR-ECC Simulator has been validated for its
effectiveness and ease of use, making it an invaluable resource for both novice
and experienced perfusionists in the medical field. [36]
Chapter 1. State of Art 1.4. VR applications in cardiology
15
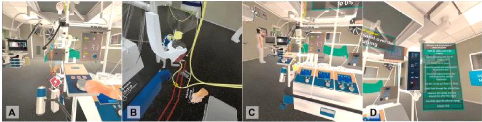
Figure 1.6: Screen captures from the virtual
reality-extracorporeal circulation (VR-ECC) simulator, featuring from
left-to-right: adjustment of the venous occluder (A), removal of the a clamp
from the arterial line (B), an overview of the heart-lung machine (C), and the
menu system by which users navigate through the simulation (D).
· vCathLab
vCathLab is an advanced medical simulation platform that uses
Virtual Reality (VR) to provide immersive and interactive training for
healthcare professionals, particularly in the field of interventional
cardiology. It allows users to practice cardiac catheterization procedures in a
realistic virtual environment, thereby enhancing their skills without the risks
associated with real procedures on patients. The platform includes authoring
tools to generate customized virtual patients and various clinical scenarios,
facilitating comprehensive and adaptable training. [37]
Figure 1.7: home page of the official vCathlab website
· Osso VR - Cardiology Modules
(with ACC collaboration)
Osso VR partnered with the American College of Cardiology
(ACC) to develop immersive left atrial appendage occlusion (LAAO) training
modules. Trainees don a VR headset (such as Meta Quest or Oculus Rift) and
rehearse step-by-step procedural workflows, including imaging control, device
manipulation, and live anatomy visualization, all within a repeatable virtual
environment. [38]
Osso VR offers trial access for educators and learners; contact
through their official site.

Chapter 1. State of Art 1.4. VR applications in cardiology
16
Figure 1.8: Image courtesy of Osso VR.
1.4.2 Comparative analysis of existing solutions and
benefits of our solution.
|
VCSim3
|
VR-ECC Simulator
|
vCathLab
|
Osso VR
|
Accessible in Daily Life
|
No
|
No
|
Yes
|
Yes
|
Equipment Cost
|
High
|
High
|
Affordable
|
Affordable-High
|
Easy Setup
|
No
|
No
|
Yes
|
Yes
|
Ease of Learning
|
Difficult
|
Moderately Difficult
|
Moderate
|
Moderate
|
Offline Functionality
|
No
|
No
|
No
|
No
|
Treat Coronary Obstructions
|
No
|
No
|
Yes
|
Yes
|
|
Table 1.1: Comparison of VR Solutions for Cardiology
Training
By analysing this table,we can notice that while several
VR-based cardiology training tools such as VCSim3, VR-ECC Simulator, vCathLab,
and Osso VR offer valuable functionalities, they also present notable
limitations. Some lack offline access or daily usability, while others require
significant financial investment or pose moderate learning difficulties.
Furthermore, only a few provide focused training on coronary obstruction
treatment. These observations highlight the need for more inclusive,
accessible, and affordable solutions that respond effectively to the real needs
of cardiology trainees and practitioners.
Our proposed solution addresses several gaps observed in
existing tools. Designed to be accessible within the daily environment of
medical learners, it combines affordability, ease of installation, and offline
functionality. With a simplified user interface, it minimizes the time needed
to get started. Most importantly, it specifically supports coronary obstruction
training,a critical yet underrepresented component in current platforms. By
focusing on inclusivity, practicality, and contextual relevance, our solution
aims to democratize cardiology training in low-resource settings.
Chapter 1. State of Art 1.4. VR applications in cardiology
17
Conclusion
Interventional cardiology is a demanding medical discipline
requiring precise technical skills and real-time decision-making. Traditional
training methods, while effective, often face challenges of cost, access, and
standardization, particularly in low and middle income countries. In this
context, virtual reality emerges as a valuable complementary tool for training
healthcare professionals. It enables learners to visualize complex procedures
in a risk-free, immersive environment particularly those involving the
treatment of coronary obstructions, which require high precision and
confidence. By simulating real-life coronary interventions, VR fosters deeper
understanding, improves procedural memory, and enhances practitioner readiness
before clinical exposure. This approach can significantly contribute to the
democratization of specialized medical education by making high-quality,
targeted training such as for coronary obstruction treatment more accessible,
flexible, and context-relevant. The observations and gaps identified in this
chapter provide a solid foundation for proposing a VR-based training solution
tailored to the specific needs of interventional cardiology.
The following chapter will present our solution through its
design and the various tools used to implement it.
18
Chapter2
Conception and technical choices
Introduction
At the beginning of creating an application, it is necessary
to formalize the preliminary steps of its development to make it more aligned
with the client's needs. This chapter presents the various phases of modeling
the proposed solution as well as the different tools and technologies used for
its implementation.
2.1 Analysis and design
This phase consists of understanding the context of the
application. It involves determining the functionalities and performance
criteria that our application must fulfil.
2.1.1 Needs analysis
Functional needs
Functional needs are the system's functionalities, they
represent the user's primary needs. Thus, through the solution, the user will
be able to:
· Select and view a healthy heart, an obstructed heart,
and/or the operating room and equipments in 3D ;
· Simulate assisted PCI or CABG on an obstructed
heart;
· Simulate autonomous PCI or CABG on an obstructed
heart; Once we have designed an administrator system, the administrator will be
able to:
· Add or modify training modules;
· Update 3D models or clinical cases;
Non-functional needs
Non-functional needs are those that characterize the system.
These are needs relating to performance and hardware type. The non-functional
needs of the solution can be listed as follows:
·
Chapter 2. Conception and technical choices 2.1. Analysis and
design
Comfortable VR experience (minimal eye strain and motion
sickness);
· Attractive and user-friendly interfaces;
· Realistic and intuitive interactions;
· Smooth and stable performance (high frame rates, low
latency, fluid animations);
· Immersive and visually accurate environment;
· Ergonomics and hardware compatibility;
2.1.2 Design
2.1.2.1 Technical design
We now enter the modelling phase. It is an essential part of
large software projects and is also useful for medium-sized and even small
projects. For this phase, we have opted for the UML (Unified Modeling Language)
modelling language which is [39] is a standard modeling language that uses
diagrams to help developers design, understand, and document software systems
and business processes. In the following sections, we reprensent our system
with both a use case diagram and a sequence diagram.
Use case diagram
The use case diagram in Figure 2.1 shows the different
actions performed by the actors. An actor represents a person, process, or
object outside the system that interacts with it.
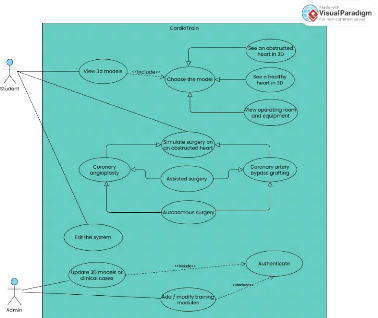
Figure 2.1: Use case diagram
19
Chapter 2. Conception and technical choices 2.1. Analysis and
design
20
Sequence diagram
The sequence diagram shows the interactions between the
system and the actors in chronological order. Figure 2.2 shows the sequence
diagram for the use case `Simulate surgery on an obstructed heart'.
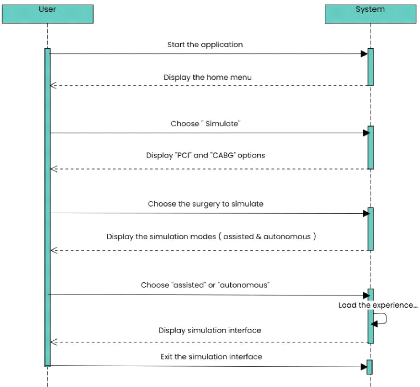
Figure 2.2: Sequence diagram for the use case "Simulate surgery
on an obstructed heart"
2.1.3 Fundamental design
The different stages of our application's development are:
· Project analysis: Understanding the needs, defining
learning objectives, features, and target users.
· 3D object modeling: Creating digital models of organs,
coronary vessels, medical tools, and the surgical environment.
· Model animation: Adding realistic movements (catheter
insertion, heartbeat, blood flow) to simulate medical procedures.
· Immersive environment assembly: Integrating the models
into a fully interactive and realistic VR scene.
·
Chapter 2. Conception and technical choices 2.2. Technical
choices
21
User Interface development: Designing menus, controls, and
feedback systems to guide the user through the simulation.
· Visual identity design: Creating the logo, selecting
colors and fonts to ensure a consistent visual branding.
· Demo testing: Conducting initial testing to evaluate
usability, flow, and relevance of the content.
· Project compilation and testing: Final technical
adjustments, debugging, and optimization for deployment.
· Performance tracking integration: Adding a system to
monitor user progress, scores, and provide feedback for learning.
2.2 Technical choices
Several technical resources were mobilised to develop the
virtual reality simulation application. These can be divided into two main
categories: on the one hand, tools dedicated to designing the 3D universe, such
as modelling and texturing software; on the other hand, those essential to the
functioning of the simulation, including a game engine, a programming language
and an SDK adapted to virtual reality.
2.2.1 Choice of 3D modelling and animation software
Blender
Blender is a free and open-source software for 3D modeling,
animation, rendering, compositing, and video editing. Highly versatile and
powerful, it is widely used across fields such as visual effects, game
development, architecture, and virtual reality. It enables the creation of
realistic or stylized 3D scenes, texturing, lighting, object and character
animation, as well as simulation of physical phenomena like smoke, fluids, and
collisions. As a cost-free solution, it stands as a strong alternative to
expensive professional software. [40]
Originally developed by the Dutch animation studio NeoGeo in
the 1990s, Blender was released to the public in 1998. After the bankruptcy of
NaN (Not a Number), the company that distributed Blender, the open-source
community rallied to buy back the software and continue its development under a
free license. Since then, Blender has been actively maintained by the Blender
Foundation and a large global community of developers and artists. Today, it is
recognized as a professional-grade tool used by both indie creators and major
studios. [41]
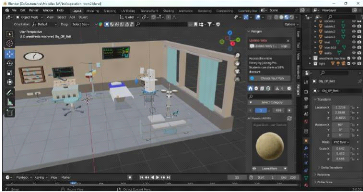
In our surgical simulation application, Blender was used to
create realistic 3D models of the human heart and simulate surgical
interactions for treating coronary obstructions. Its sculpting, rigging, and
animation tools allowed precise modeling, procedure animation, and immersive
visual integration. While alternatives like Autodesk Maya, 3ds Max, Cinema 4D,
and ZBrush exist, Blender was chosen for its free access, active community,
frequent updates, and seamless compatibility with Unity, making it ideal for
efficiently producing realistic biomedical models.
Chapter 2. Conception and technical choices 2.2. Technical
choices
22
Figure 2.3: Operating room design in Blender 2.2.2 Choice
of game engine and programming language
Unity & C-Sharp (C#)
Unity, developed by Unity Technologies, is a widely used
cross-platform engine for creating interactive 2D and 3D applications,
including VR and AR simulations. Its robust tools for rendering, physics,
scripting, and asset management, along with multi-platform deployment, made it
ideal for our project. We used Unity 2020.3.41f1 (LTS) for stability and
long-term support, leveraging C#, Unity's native language, which offers clean
object-oriented syntax, automatic memory management, and seamless integration
with Unity's API. This enabled us to efficiently implement VR interactions,
simulate surgical procedures, design user interfaces, and maintain a
structured, maintainable code-base. The engine also allowed seamless
integration with 3D assets created in Blender and facilitated real-time testing
of surgical scenarios. Compared to alternatives like Unreal Engine (C++) and
Godot (GDScript), Unity provided the best combination of flexibility,
performance, and mature VR support, ensuring a smooth development process for
our immersive cardiology training software.
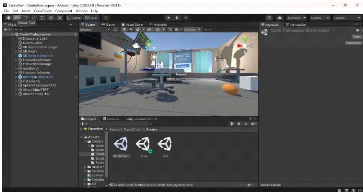
Figure 2.4: Using the Unity3D engine to create the VR
experience
Chapter 2. Conception and technical choices 2.2. Technical
choices
23
2.2.3 IDE
To write, debug, and manage our C# scripts within Unity, we
used Visual Studio Community 2017. This free, full-featured IDE developed by
Microsoft is officially supported by Unity and offers excellent integration
with it, including IntelliSense, debugging tools, error tracking, and project
organization. Its lightweight setup and reliable performance made it an ideal
choice for our workflow, especially in the context of Unity 2020.3.41f1.
Other alternatives like JetBrains Rider, Visual Studio Code,
or MonoDevelop exist, but Visual Studio Community stands out due to its deep
Unity support, professional-grade features, and longstanding stability. Its
compatibility with Unity packages and ease of configuration for VR scripting
made it especially valuable during our project.
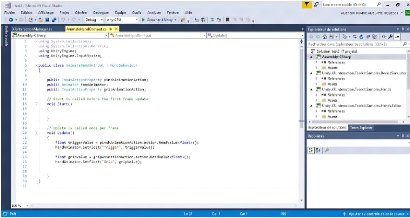
Figure 2.5: Script for animating the user's hands written in
Visual Studio 2017 2.2.4 Choice of SDK and frameworks for
YR
· SDK
The Software Development Kit we used is Oculus XR
Plugin[43], a comprehensive set of tools, libraries, and resources
provided by Unity for developers who want to create virtual reality (VR)
experiences for Oculus headsets, including Quest, Quest 2, Quest 3, and Rift
devices. It offers robust support for device tracking, controller input, hand
tracking, haptic feedback, and platform-specific optimizations, making it
easier to build immersive and responsive VR environments. Although primarily
designed for Oculus hardware, it can be combined with Unity's XR framework to
support cross-platform VR development. The choice of the Oculus XR Plugin in
our project is due to its native compatibility with Oculus devices, ensuring
precise interactions and smooth locomotion. It also excels in delivering an
intuitive and immersive user experience, which was essential for our VR
application.
· Frameworks
We used the Unity XR Interaction Toolkit, a
flexible framework designed to simplify the creation of VR and AR experiences
by providing ready-to-use components for interactions, locomotion, and user
interface control [42]. It allows developers to define interactive objects
(which users can grab, tap, or manipulate) and interactors, which represent
input devices such as VR
Chapter 2. Conception and technical choices 2.3. Development
methodology
24
controllers or hand tracking. In the context of our project,
this toolkit proved essential for enabling intuitive manipulation of surgical
tools.
2.2.5 Others softwares Adobe Illustrator
Adobe Illustrator is a widely recognized vector graphics
creation software in professional environments. Part of the Adobe suite, it can
be used independently or in conjunction with Photoshop, offering powerful
vector drawing tools. Vector images, composed of curves defined by mathematical
formulas, have the advantage of being resolution-independent, meaning they
retain their quality even when enlarged. Illustrator is suitable for creating
printed documents as well as illustrations for the web, such as logos and
posters. It offers numerous features designed to enhance productivity. For
creating the logo of our application, we chose to use Adobe Illustrator CC
2020. Figure 2.6 shows the software interface during its use for designing the
logo.
Figure 2.6: Adobe Illustrator interface screenshot
Adobe Photoshop
Adobe Photoshop is a computer-assisted editing, processing,
and drawing software, introduced in 1990 and available for MacOS and Windows
since 1992. Developed by Adobe, it is primarily used for digital photo
processing and also allows for creating images from scratch. Photoshop mainly
works with raster images, which are composed of a grid of points called pixels.
The advantage of these images is their ability to reproduce subtle color
gradations.
2.3 Development methodology
The software was developed using an Iterative and
Incremental Development approach, enabling gradual building, testing,
and refinement. This methodology is especially suitable for projects involving
3D modeling, VR integration, and interactive software. The main stages of
development are
Chapter 2. Conception and technical choices 2.3. Development
methodology
25
outlined below:
· Specification definition: The project started by
defining application requirements and objectives, detailing expected features,
user interactions, and the scope of simulated surgical procedures. This stage
provided a solid foundation for all subsequent development activities.
· Project planning and task breakdown: The project was
divided into smaller, manageable tasks, each producing deliverables that
contributed to the overall application. This approach enabled effective
progress tracking, task prioritization, and iterative improvements.
· Information gathering: Medical accuracy was ensured by
collecting information from online sources, cardiology students, and
professional cardiologists. This research informed the VR representation of
operating procedures and surgical workflows.
· Scenario and workflow development: Application
scenarios and surgical procedure scripts were created to define user
interactions, procedural sequences, and expected behaviors within the virtual
environment.
· Modeling and asset creation
- Installation and setup of Blender and Adobe
Photoshop - Modeling, texturing, and basic animation of 3D
objects - Exporting 3D models for integration into Unity
· Integration and Incremental Development in Unity
- Design of the logo and graphic charter to
ensure visual consistency;
- User interface (UI) design and layout;
- Installation of Unity and required SDKs;
- Importation of characters and 3D models;
- Creation of different scenes and VR camera
configuration;
- Learning and applying C# to implement
interactive features;
- Writing scripts to manage events and
functionalities;
- Development of incremental features and
functionalities;
- Deployment on the Oculus Quest 3 headset for
iterative testing;
· Testing, validation, and refinement: Each increment of
the application was tested to ensure correct functionality, usability, and
immersion. Feedback from testing guided adjustments and improvements, allowing
the application to evolve gradually toward the final version.
Conclusion
This chapter has been devoted to presenting the proposed
solution, detailing both its design and all the tools used to implement it. We
have also described the various stages of the development process, providing an
overview of the approach taken to bring the application to fruition. The next
chapter will be dedicated to illustrating this solution by presenting some of
the application's key interfaces.
26
Chapter3
Presentation of the solution and discussions
Introduction
After our solution was implemented, several tests were
carried out to verify that it met the client's needs and complied with the
planned non-functional requirements. This chapter presents some interfaces
captured during the tests carried out on the solution, and a discussion of the
shortcomings of the present work.
3.1 Presentation of the software
3.1.1 Visual Identity 3.1.1.1 Main logo
design
The CardioTrain logo illustrates the alliance between
medicine and innovation. The virtual reality headset symbolises immersive
learning, while the electrocardiogram curve joins a heart, evoking life and
cardiology. Understated and modern, it reflects the ambition to train
differently in order to provide better care.

Figure 3.1: CardioTrain Logo
Chapter 3. Presentation of the solution and discussions 3.1.
Presentation of the software
27
3.1.1.2 Color palette and visual harmony
The color palette that we have created for CardioTrain
reflects the dual essence of healthcare and technology. It contains:
· The dominant teal shades (#27828C,
#278793, #3F9C94) which are the main colours and evoke calm,
confidence and scientific precision, essential values in the medical field.
· The brighter blue (#048ABF) that
introduces a sense of innovation and vitality, symbolizing the energy of
learning and progress.
· The light gray (#F2F2F2) that ensures
visual balance and clarity, providing a neutral background that enhances
readability and highlights the main elements.
Together, these colors create a serene yet dynamic atmosphere
that mirrors the mission of CardioTrain : offering an immersive, safe, and
forward-thinking learning experience in cardiology.
Figure 3.2: CardioTrain Color Palette
3.1.1.3 Logo variations and adaptations
To ensure flexibility and visual consistency across all
communication materials, the CardioTrain logo was designed in multiple versions
adapted to various backgrounds.
The primary version, featuring the teal gradient, embodies
the full identity of the brand and is mainly used for digital and presentation
purposes.
The monochrome versions, in black and white, ensure
readability and contrast when color reproduction is limited or when simplicity
is preferred, such as on official documents or technical assets.
Finally, the inverted version allows seamless integration on
dark or photographic backgrounds while maintaining the logo's clarity and
impact.
These variations guarantee that the CardioTrain identity
remains recognizable and professional across all contexts from digital media to
print and immersive environments.

Chapter 3. Presentation of the solution and discussions 3.1.
Presentation of the software
Figure 3.3: CardioTrain logo variations 3.1.1.4 Logo
usage guidelines and restrictions
To preserve the integrity and visual coherence of the
CardioTrain identity, the following rules must be strictly observed. It is
strictly prohibited to:
· Modify the logo colors or apply non-approved color
variations.
· Rotate, tilt, flip, distort, stretch, compress, or
alter the logo's proportions or original orientation in any way.
· Add special effects such as shadows, glow, gradients,
or textures.
· Place the logo on a busy or overly contrasted
background that compromises its readability.
· Add any unapproved elements to the logo (extra text,
icons, or slogans).
· Use unofficial, recreated, or outdated versions of the
logo.
· Display the logo below the minimum readable size
(recommended minimum width: 5cm / 189 px).
These restrictions ensure that the CardioTrain logo remains
consistent, professional, and immediately recognizable across all
applications.
3.1.1.5 Visual applications

Figure 3.4: A few examples of the logo in use
28
Chapter 3. Presentation of the solution and discussions 3.1.
Presentation of the software
3.1.2 Software interfaces
· Choice of experience
When the software starts up, a splash screen is shown before
the home interface where the user must choose the experience they wish to
perform. At this stage, the user can choose between viewing 3D models (healthy
heart, obstructed heart or operating room) and performing one of the surgical
procedures in assisted or autonomous mode.
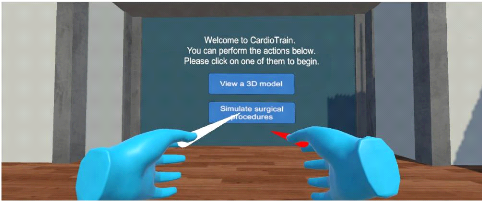
Figure 3.5: Home interface
· Selecting and choosing an instrument
The user sees all the instruments laid out on a medical
trolley. When the user hovers over each instrument with the joystick pointer,
the corresponding name is displayed, allowing it to be clearly identified. Once
the desired instrument has been identified, the user can select it using the
joystick to use it in the experiment.
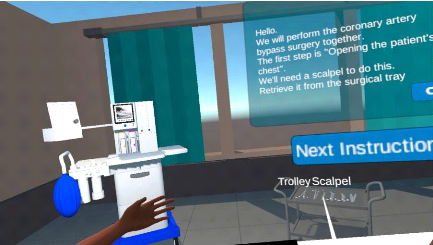
Figure 3.6: Selecting and choosing an instrument
29
· Chapter 3. Presentation of the solution and discussions
3.1. Presentation of the software
30
Assisted experience flow VS Autonomous experience
flow
- Assisted mode: The software provides
step-by-step instructions that guide the user throughout the simulation. Each
task is presented in a specific order to ensure proper understanding and
execution. This mode is ideal for beginners or users who prefer a structured
approach.
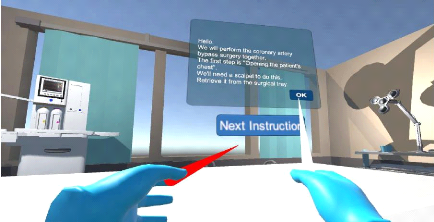
Figure 3.7: Assisted CABG
- Autonomous mode: The user explores and
completes the simulation freely, without guided instructions. This mode
encourages self-paced learning and allows for more independent practice, ideal
for reinforcing previously acquired knowledge.
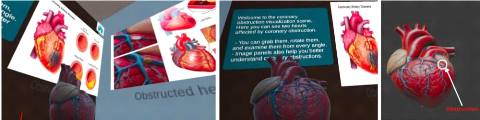
· 3D models and room exploration
Users can move freely around the virtual room and interact
with detailed 3D anatomical models. When they hover over an element, text
descriptions appear to provide additional information. They can also observe a
healthy heart and a blocked heart to better understand the anatomical
differences and medical implications.
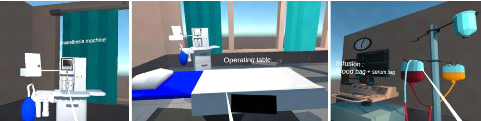
Figure 3.8: some 3D operating room exploration screenshots
Chapter 3. Presentation of the solution and discussions 3.2.
Challenges encountered and solutions
31
Figure 3.9: some 3D hearts exploration screenshots
3.2 Challenges encountered and solutions
During the development of the project, we faced several
challenges both at the technical and design levels.
The 3D modeling phase raised particular difficulties,
especially with highly complex medical equipment such as the heart-lung machine
and the anesthesia machine. Due to their intricate structures, these models
were downloaded from Sketchfab instead of being modeled from blender. In
addition, 3D models significantly affected both application performance and the
overall build size, making the application heavier than expected. In order to
address this, we optimized the models by reducing polygon counts, simplifying
textures, and selectively replacing certain components with lighter assets,
which allowed us to preserve realism while maintaining smooth execution.
Another issue arose when importing models and animations from
Blender to Unity. In several cases, the process resulted in visual glitches,
unexpected physical collisions, or partial loss of animations. These problems
were progressively fixed by carefully reviewing the import settings and testing
different export formats until the most stable configuration was identified.
At one stage, certain objects started moving unexpectedly
within the scene. After investigation, it was discovered that this was caused
by the simultaneous presence of both mesh colliders and box colliders on the
same objects. Restarting the debugging process from the beginning allowed us to
isolate the problem and resolve it by cleaning up redundant colliders.
We also faced challenges with the choice of SDK, as it
directly influenced the Unity version required for proper compatibility. This
constraint sometimes limited the features we could use and adapting to it
required additional testing and adjustments.
Finally, simulating transitions between physiological states
proved to be a significant challenge. Modeling the shift from pathological to
normal condition, such as restoring coronary blood flow after an intervention
required more than static changes. To ensure immersion, we tried to synchronize
animations, shaders, and physiological parameters, allowing for smooth and
medically plausible transitions.
However, by combining online researches, trial-and-error
experimentation, and the insightful guidance of our supervisor, we were able to
identify the right resources and effectively overcome these obstacles.These
experiences not only strengthened our technical skills, but also emphasized the
importance of patience, iteration, and systematic debugging in XR
development.
Chapter 3. Presentation of the solution and discussions 3.3.
Discussion
32
3.3 Discussion
The developed prototype provides two complementary learning
modes: a guided experience and an autonomous experience of PCI and CABG
procedures, both designed to address coronary obstructions. Through this
application, learners are immersed in a simulated operating room equipped with
the necessary instruments, enabling them to become familiar with operative
techniques, understand the role of each tool, and progressively develop
surgical reflexes in a risk-free, immersive setting. This approach enhances
experiential learning and bridges the gap between theoretical knowledge and
practice.
Nevertheless, the current version of the prototype presents
several limitations. First, the graphical quality, while functional, lacks the
photorealism of advanced commercial platforms which integrate highly detailed
anatomical models and lighting effects. Second, the system does not yet include
complex autonomous scenarios with unexpected complications, which are essential
for preparing students for the unpredictability of real-world interventions.
Third, the absence of haptic feedback reduces the ability to practice fine
motor skills and the tactile dimension of surgery. Fourth, the software is
limited to single-user mode and does not support collaborative training
sessions, whereas some commercial systems already integrate multi-user
experiences.Fifth, the current version does not include detailed assessment
tools such as performance metrics, error tracking, or progression analysis,
while commercial solutions often provide comprehensive dashboards that enable
trainers to objectively evaluate and track learners' skills. Finally,
optimization issues such as build size, performance drop with complex assets,
and limited device compatibility still restrict large-scale deployment.
Despite these limitations, the proposed solution demonstrates
notable strengths. Its accessible cost makes it considerably more affordable
than many commercial VR simulators, which often require expensive licenses and
specialized hardware. Moreover, its current ability to operate offline ensures
that learners can benefit from the training experience without relying on
constant internet connectivity.Although it has not yet achieved the
sophistication of international benchmarks, it provides a promising, adaptable,
and scalable foundation to advance cardiology training through im-mersive
technologies.
Conclusion
This chapter demonstrates that the prototype provides an
immersive, interactive environment for cardiology training, enabling learners
to develop surgical reflexes through guided and autonomous experiences. The
development process exposed technical and design challenges, from complex 3D
models to smooth physiological transitions, strengthening our optimization and
iterative refinement skills. Although limitations remain compared to advanced
commercial systems such as absence of haptic feedback, assessment tools and
complex scenarios, the prototype's accessible cost, offline functionality, and
user-friendly design make it a promising, adaptable, and scalable foundation
for cardiology education. Overall, the chapter shows that the solution
represents a meaningful step toward bridging the gap between theoretical
knowledge and practical skills in immersive medical training.
33
General conclusion and perspectives
This work is part of a dynamic of pedagogical innovation
through the use of virtual reality. We have designed and developed an immersive
application prototype that simulates two major surgical procedures used in the
treatment of coronary obstructions: Coronary Artery Bypass Grafting (CABG) and
Percutaneous Coronary Intervention (PCI). This solution aims to offer learners
a safe, interactive, and autonomous environment to become familiar with
surgical techniques, instruments, and the overall process of these
procedures.
One of the main strengths of our application is its ability to
combine guided assistance with autonomous learning, serving as a complementary
tool to support the practical preparation of cardiology students in conjunction
with existing training methods. It is expected to provide added value to
surgical education, as suggested by studies and tests conducted in several
countries [46, 47], by allowing learners to explore, practice, and reinforce
their knowledge in a safe, risk-free environment.
The design process we adopted was based on a rigorous analysis
of user needs, followed by a technical implementation using tools such as
Blender for 3D modeling, Unity for interactive development, and a suitable SDK
for VR integration.
Although this first version can still be improved particularly
in terms of graphical realism and scenario diversity,it opens the door to
promising developments. Future developments will aim to enhance graphical
realism, incorporate complex autonomous scenarios with unexpected
complications, integrate haptic feedback to support fine motor skills, enable
collaborative multi-user experiences, and implement detailed assessment tools
such as performance metrics and error tracking. Optimization challenges,
including build size, performance with complex assets, and broader device
compatibility, will also be addressed. By tackling these limitations, the
application can become a more immersive, educationally effective, and widely
deployable tool, supporting the ongoing digital transformation of cardiology
training while complementing existing teaching methods.
34
Bibliography
[1] Manuel indispensable pour Unity, 18 03 2016, Julien
Faujanet.
[2] A taxonomy of mixed reality visual displays,Milgram, P.,
& Kishino, F. (1994).
[3] A structural equation modeling investigation of the
emotional value of immersive virtual reality in education. Education Tech
Research Dev 66, 1141-1164 (2018).
https://doi.org/10.1007/s11423-018-9581-2
, Makransky, G., Lilleholt, L.
https://link.springer.com/article/10.1007
/s11423-018-9581-2
[4] Learning Blender: "A Hands-On Guide to Creating 3D
Animated Characters", Olivier Villar, 2014
[5] Workflow for Percutaneous Coronary Intervention With Optical
Coherence Tomography-Guidance: MAXing the MLD? Circ Cardiovasc Interv. 2022
Nov;15(11):882-883. doi: 10.1161/CIRCINTERVENTIONS.122.012608. Epub 2022 Nov
15. PMID: 36378740, Razzouk L, Attubato MJ.
[6] Mise en place d'une application mobile pour la
rééducation en réalité virtuelle: cas de simulation
d'imagerie motrice, Bachelor's thesis, University of Abomey-Calavi, IFRI,
Benin, 2023, Oloufèmi Adéwoumi Lazare Jean-deluxe FAGBOHOUN.
[7] Application de simulation médicale en
réalité virtuelle: cas de l'appendicectomie, Bachelor's thesis,
University of Abomey-Calavi, IFRI, Benin, 2019, Afis Mahoutin Malick KOUSSE.
35
Webography
[8] World Health Organization,
https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1,
Last visit: 03 May 2025,10:55 ,
[9] Coronary artery disease,
https://www.mayoclinic.org/diseases-conditions/coron
ary-artery-disease/symptoms-causes/syc-20350613, Last visit: 03 May 2025, 14:55
,
[10] World Health Organization,
https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1,
Last visit: 03 May 2025, 10:55.
[11] World Health Organization, Regional Office for Africa,
https://www.afro.who.int/hea
lth-topics/cardiovascular-diseases, Last visit: 11 May 2025, 09:43.
[12] World Heart Federation, *World Heart Report 2023*,
https://world-heart-federation
.org/wp-content/uploads/World-Heart-Report-2023.pdf, Last visit: 11 May 2025,
09:45.
[13] World Health Organization, *Noncommunicable Diseases
Country Profile: Benin*, https:
//www.afro.who.int/sites/default/files/2023-08/Benin.pdf, Last visit: 11 May
2025, 09:47.
[14] Sanofi IMPACT, *Tackling Non-Communicable Diseases in
Benin*,
https://www.impact
.sanofi/news/tackling-non-communicable-diseases-in-benin, Last visit:
11 May 2025, 09:48.
[15] Tossou, O. A. et al., *Les maladies cardiovasculaires
à l'Hôpital de Zone de Suru-Léré*, Open Journal of
Internal Medicine, vol. 11, pp. 202-210, 2021.
https://www.scirp.org/journal/
paperinformation.aspx?paperid=110241, Last visit: 11 May 2025, 09:50.
[16] Percutaneous Coronary Intervention (PCI),
https://www.yalemedicine.org/condition
s/percutaneous-coronary-intervention-pci, Last visit: 18 june 2025, 18:50.
[17] ACC/AHA Guidelines for Percutaneous Coronary
Intervention (Revision of the 1993 PTCA Guidelines),
https://www.ahajournals.org/doi/10.1161/01.cir.103.24.3019,
Last visit: 12 july 2025, 11:57.
[18] What equipment is used in angioplasty?,
https://www.tjmedtech.com/What-equipmen
t-is-used-in-angioplasty-id49296876.html,Lastvisit: 12 july 2025, 12:37.
[19]
36
Catheters used in PCI ,
https://www.medtronic.com/en-ca/healthcare-professionals/products/cardiovascular.html#aq=%40pagetype%3D%22product-model%22&cq=%40products_category%3D%22Cardiovascular%22%20OR%20%40ontol
ogy_isa%3D%22Cardiovascular%22, Last visit: 17 july 2025, 22:20.
[20] Coronary Artery Surgery,
https://www.ncbi.nlm.nih.gov/books/NBK562187/,
Last visit: 19 july 2025, 07:27.
[21] Coronary Artery Surgery,
https://www.fmptr.com/Instruments-for-Coronary-Ar
tery-Bypass-Graft--CABG--Surgery--An-In-Depth-Guide, Last visit: 19 july 2025,
08:08.
[22] Coronary Artery Surgery Procedure,
https://stanfordhealthcare.org/medical-tr
eatments/c/coronary-artery-bypass-graft-surgery/procedures/during.html, Last
visit: 19 july 2025, 08:27.
[23] Coronary Artery Surgery Complications,
https://stanfordhealthcare.org/medical-treatments/c/coronary-artery-bypass-graft-surgery/complications.html,
Last visit: 19 july 2025, 08:45.
[24] Bori Bata, K., Sonou, A., Dohou, H., Aïkpon, D.,
Agbo, M., et al. (2023). Acute Aortic Dissection at the Cardiology Clinic to
the University National Hospital Hubert Koutoukou Maga of Cotonou (BENIN).
International Journal of Cardiovascular and Thoracic Surgery, 9(6), 71-76.
https://doi.org/10.11648/j.ijcts.20230906.11
,
https://www.sciencepg.com/arti
cle/10.11648/j.ijcts.20230906.11, Last visit: 19 july 2025, 12:24.
[25] BMC Medical Education: Effects of simulation in
improving the self-confidence of student nurses in clinical practice: a
systematic review ,
https://bmcmededuc.biomedcentral.com
/articles/10.1186/s12909-023-04793-1, Last visit: 25 july 2025, 23:42.
[26] BMC Medical Education: Stress responses in high-fidelity
simulation and standard simulation training among medical students ,
https://bmcmededuc.biomedcentral.com/articles/
10.1186/s12909-023-04101-x, Last visit: 25 july 2025, 23:53.
[27] Yount KW, Yarboro LT, Narahari AK, Ghanta RK, Tribble CG,
Kron IL, Kern JA, Ailawadi G. Outcomes of Trainees Performing Coronary Artery
Bypass Grafting: Does Resident Experience Matter? Ann Thorac Surg. 2017
Mar;103(3):975-981. doi: 10.1016/j.athoracsur.2016.10.016. Epub 2017 Jan 26.
PMID: 28131424. ,
https://pubmed.ncbi.nlm.nih.gov/28131424/,
Last visit: 26 july 2025, 06:28.
[28] Patrick WL, Iyengar A, Han JJ, Mays JC, Helmers M, Kelly
JJ, Wang X, Ghoreishi M, Taylor BS, Atluri P, Desai ND, Williams ML. The
learning curve of robotic coronary arterial bypass surgery: A report from the
STS database. J Card Surg. 2021 Nov;36(11):4178-4186. doi: 10.1111/jocs.15945.
Epub 2021 Aug 29. PMID: 34459029; PMCID: PMC9128069. ,
https://pubmed.ncbi.nlm.ni
h.gov/34459029/, Last visit: 26
july 2025, 06:41.
[29] L'essentiel sur...La réalité virtuelle ,
https://www.cea.fr/comprendre/Pages/nouvelle
s-technologies/essentiel-sur-realite-virtuelle.aspx, Last visit: 26 july 2025,
08:46.
[30]
37
Slater, M. (2003). A note on presence terminology. Presence
Connect. ,
https://www.resear
chgate.net/publication/242608507_A_Note_on_Presence_Terminology,
Last visit: 26 july 2025, 08:55.
[31] Virtual reality system helps surgeons, reassures patients ,
https://med.stanford.edu
/medicalgiving/news/virtual-reality-system-helps-surgeons-reassures-patients.html,
Last visit: 26 july 2025, 09:18.
[32] Seymour NE, Gallagher AG, Roman SA, O'Brien MK, Bansal
VK, Andersen DK, Satava RM. Virtual reality training improves operating room
performance: results of a randomized, double-blinded study. Ann Surg. 2002
Oct;236(4):458-63; discussion 463-4. doi: 10.1097/00000658200210000-00008.
PMID: 12368674; PMCID: PMC1422600. ,
https://pmc.ncbi.nlm.nih.gov
/articles/PMC1422600/?pStoreID=epp, Last visit: 27 july 2025, 09:05.
[33] The effectiveness of virtual and augmented reality in
health sciences and medical anatomy Christian Moro, Zane tromberga, Athanasios
Raikos, Allan Stirling ,
https://anatomypubs.
onlinelibrary.wiley.com/doi/10.1002/ase.1696, Last visit: 27 july 2025,
09:56.
[34] Ageing and Dementia Research Centre (ADRC) and Alzheimer's
Research UK launches immer-sive VR dementia training ,
https://blogs.bournemouth.ac.uk/research/2019/06/1
2/ageing-and-dementia-research-centre-adrc-and-alzheimers-research-uk-launches-immersive-vr-dementia-training/,
Last visit: 27 july 2025, 10:30.
[35] VR-NRP: A Virtual Reality Simulation for Training in the
Neonatal Resuscitation Program. Mustafa Yalin Aydin, Vernon Curran, Susan
White, Lourdes Pena-Castillo, Oscar Meruvia-Pastor ,
https://arxiv.org/abs/2406.15598,
Last visit: 27 july 2025, 10:44.
[36] Virtual reality simulation as a training tool for
perfusionists in extracorporeal circulation: Establishing face and
content validity. ,
https://www.jtcvstechniques.org/article/S2666-2507(23)00198-0/fulltext,
Last visit: 27 july 2025, 22:14.
[37] vCathLab website ,
https://vcathlab.com/, Last visit:
29 july 2025, 16:22.
[38] Cardiologist-approved VR for interventional procedures
headed to ACC.24 ,https: //
cardiovascularbusiness.com/topics/clinical/structural-heart-diseas
e/cardiologist-approved-vr-interventional-procedures-headed-acc24?, Last visit:
30 july 2025, 10:27.
[39] What is Unified Modeling Language (UML)? ,
https://www.visual-paradigm.com/gui
de/uml-unified-modeling-language/what-is-uml/, Last visit: 02 august 2025,
21:42.
[40] Blender's official site ,
https://www.blender.org/, Last
visit: 03 august 2025, 01:32.
[41] Blender's History ,
https://www.blender.org/about/history/,
Last visit: 03 august 2025, 01:39.
[42] XR Interaction Toolkit Documentation ,
https://docs.unity3d.com/Packages/com.un
ity.xr.interaction.toolkit@3.2/manual/index.html, Last visit: 03 august 2025,
03:09.
[43]
38
About the Oculus XR Plugin ,
https://docs.unity3d.com/Packages/com.unity.xr.o
culus@4.5/manual/index.html, Last visit: 03 august 2025, 04:11.
[44] Communiqué 1 - Probatoire Cardio 2025 ,
https://fr.scribd.com/document/88535505
7/Communique-1-Probatoire-Cardio-2025, Last visit: 14 september 2025, 09:13.
[45] Annuaire des statistiques UAC de l'année
académique 2019-2020 ,
https://www.research
gate.net/publication/366719572_Annuaire_des_statistiques_UAC_de_l%27an
nee_academique_2019-2020, Last visit: 14 september 2025, 09:17.
[46] Effectiveness of Immersive Virtual Reality in Surgical
Training--A Randomized Control Trial ,
https://www.joms.org/article/S0278-2391(17)31250-8/abstract,
Last visit: 16 september 2025, 11:12.
[47] Virtual Reality Training Improves Operating Room
Performance ,
https://pmc.ncbi.nlm.n
ih.gov/articles/PMC1422600/,
Last visit: 16 september 2025, 11:32.
39
Contents
Dedication ii
Acknowledgements iii
Résumé iv
Abstract iv
iv
v
List of Figures vi
List of Tables vii
List of Acronyms viii
Glossary ix
Introduction 2
1 State of Art 4
Introduction 4
1.1 Coronary artery diseases 4
1.1.1 Overview 4
1.1.2 Coronary artery disease's treatments 5
1.2 Cardiology training issues 8
1.2.1 Current methods of training cardiology students with
contextual focus on Benin
8
1.2.2 Limitations of the theoretical approach alone 8
1.2.3 Complication and error rates in initial coronary surgery
experiences 9
1.2.4 Existing digital solutions (Excluding immersive
technologies) 9
1.3 Immersive technologies in the medical field 11
1.3.1 Virtual Reality as a key immersive technology in medical
training 11
1.3.1.1 Types of Virtual Reality experiences in medical education
12
1.3.1.2 Tools and equipment in VR training 12
1.3.1.3 Modalities of use in medical education 12
1.3.2 Pedagogical benefits and cognitive impacts of immersive
technologies 13
1.4 VR applications in cardiology 13
1.4.1 Existing projects and tools in cardiology training 13
40
1.4.2 Comparative analysis of existing solutions and benefits of
our solution. . . . 16
Conclusion 16
2 Conception and technical choices 18
Introduction 18
2.1 Analysis and design 18
2.1.1 Needs analysis 18
2.1.2 Design 19
2.1.2.1 Technical design 19
2.1.3 Fundamental design 20
2.2 Technical choices 21
2.2.1 Choice of 3D modelling and animation software 21
2.2.2 Choice of game engine and programming language 22
2.2.3 IDE 23
2.2.4 Choice of SDK and frameworks for VR 23
2.2.5 Others softwares 24
2.3 Development methodology 24
Conclusion 25
3 Presentation of the solution and discussions
26
Introduction 26
3.1 Presentation of the software 26
3.1.1 Visual Identity 26
3.1.1.1 Main logo design 26
3.1.1.2 Color palette and visual harmony 27
3.1.1.3 Logo variations and adaptations 27
3.1.1.4 Logo usage guidelines and restrictions 28
3.1.1.5 Visual applications 28
3.1.2 Software interfaces 29
3.2 Challenges encountered and solutions 31
3.3 Discussion 32
Conclusion 32
Conclusion 33
Bibliography 34
Webography 35
Contents 39
41
| 


