|
REPUBLIQUE DU CAMEROUN
Paix - Travail - Patrie

------------------------
UNIVERSITE DE YAOUNDE I
------------------------
FACULTE DE MEDECINE ET DES
SCIENCES BIOMEDICALES
-------------------------
AN ASSESSMENT OF ADHERENCE TO ANTIHYPERTENSIVE
TREATMENT AND ASSOCIATED FACTORS IN PATIENTS AT THE YAOUNDE GENERAL
HOSPITAL
Presented by:
CHIABI ROLAND MUNTOH
7TH YEAR PHARMACY STUDENT
Thesis Presented and Defended Publicly in Partial
Fulfilment of the Requirements for the Award of a Pharmaciae Doctor (Pharm.D.)
Degree
CO-SUPERVISOR
Dr. TEMBE Estella épse FOKUNANG
Senior Lecturer of Clinical Pharmacology
SUPERVISOR
Prof. MENANGA Alain Patrick
Associate Professor of Cardiology
Academic year: 2017-2018
TABLE OF CONTENT
PREFACE
ii
DEDICATION
iii
ACKNOWLEDGEMENTS
iv
LIST OF ADMINISTRATIVE AND ACADEMIC STAFF OF THE
FACULTY OF MEDICINE AND BIOMEDICAL SCIENCES FOR THE 2017/2018 ACADEMIC YEAR
v
GALEN'S OATH
xvi
ABSTRACT
xvii
RESUME
xix
LIST OF FIGURES
xxi
LIST OF TABLES
xxii
LIST OF ABBREVIATIONS/ACRONYMS/SYMBOLS
xxiii
CHAPTER
I: INTRODUCTION
1
I.1 BACKGROUND AND RATIONALE
1
I.2 RESEARCH QUESTION
4
I.3 RESEARCH HYPOTHESIS
4
I.4 OBJECTIVES
4
CHAPTER
II: LITERATURE REVIEW
5
CHAPTER
III: MATERIALS AND METHOD
50
CHAPTER
IV: RESULTS
59
CHAPTER
V: DISCUSSION
75
CHAPTER
VI: CONCLUSION AND RECOMMENDATIONS
81
CHAPTER VII:
REFERENCES
84
CHAPTER
VIII: APPENDIX
97
PREFACE
DEDICATION
This scientific project is dedicated to my parents.
ACKNOWLEDGEMENTS
I thank GOD ALMIGHTY for His unceasing love, for keeping
strong and healthy and for His numerous graces shown to me throughout these
years of pharmacy training.
This work will not have been a success without the
contributions of the following people:
Ø My supervisor, Prof MENANGA Alain, for his continuous
support, patience, motivation and immense knowledge. His guidance helped me
throughout the research period and also during the writing of this thesis. I
could not have imagined having a better advisor and mentor for my end of course
thesis.
Ø My cosupervisor, Dr. TEMBE Estella, for her
insightful comments and encouragements but also for the hard questions which
motivated me to widen my research from various perspectives! Thank you Doctor
for being a mentor for me and for sharing your experiences with me throughout
these years. I am forever grateful.
Ø The cardiologists and the nurses of the external
consultation unit, who facilitated my integration into the healthcare team.
Without their precious support it would not have been possible to conduct this
research.
Ø All the participants in my study, who willingly
spared their precious time to answer my questions.
Ø All the lecturers of the Faculty of Medicine and
Biomedical Sciences (FMBS) for grooming me throughout these years of
pharmaceutical studies.
Ø My parents for all the sacrifices, encouragements and
support they have made on my behalf. Your prayers for me was what sustained me
this far.
Ø My brothers, CHIABI Edmond, CHIABI Valery and CHIABI
Leslie, and the rest of my family for their support and the love they have
always been showing me.
Ø Dr. NGANGUE NSEKE Rose, Dr. ABONG BWEMBA Therese and
Dr. KIMA Tessa for their mentorship, assistance, and dedicated involvement in
one level or another in my training. I would like to thank you very much for
your support, advice and understanding throughout these years.
Ø All my classmatesand friends for the love, the
friendship, the support, the stimulating scientific discussions, the fun and
the patience.
Ø The Director of the Yaounde General Hospital for
granting me the authorization to pursue this research.
Ø Mr TCHUISSEU Frederic for the statistical
analysis.
Ø All those who contributed in the elaboration of this
work.
LIST OF ADMINISTRATIVE AND
ACADEMIC STAFF OF THE FACULTY OF MEDICINE AND BIOMEDICAL SCIENCES FOR THE
2017/2018 ACADEMIC YEAR
|
S/N
|
1. ADMINISTRATIVE PERSONNEL
|
|
1.
|
Pr ZE MINKANDE Jacqueline
|
Dean
|
|
2.
|
Pr NTSAMA ESSOMBA Claudine Mireille
|
Vice- Dean in charge of programs and academic activities
follow-up
|
|
3.
|
Pr Gloria Enow ASHUNTANTANG
|
Vice-Dean in charge of School, Statistics and Students
follow-up
|
|
4.
|
Pr KAMGNO Joseph
|
Vice- Dean in charge of Research and Cooperation
|
|
5.
|
Mr MEKA Gaston
|
Director of Administrative and Financial affairs
|
|
6.
|
Pr BENGONDO MESSANGA Charles
|
Director of Academic, School and Research affairs
|
|
7.
|
Pr MOUAFO TAMBO Faustin
|
General Coordinator of Specialisation Cycle
|
|
8.
|
Mr. ADAMOU
|
Chief of Financial Service
|
|
9.
|
Dr SAMBA Odette NGANO ép. TCHOUAWOU
|
Chief of General Administration and Personnel Service
|
|
10.
|
Mme ASSAKO Anne DOOBA
|
Chief of Service : Certificates
|
|
11.
|
Dr NSEME Eric
|
Chief of Service : School and Statistics
|
|
12.
|
M. MPACKO NGOSSO Charles Romuald
|
Chief of Service : Materials and Maintenance
|
|
13.
|
Mme FROUISSOU née MAME Marie-Claire
|
Interim Chief of the Library
|
|
14.
|
Mme ANDJISSILE ENAM Suzel Chanel
|
Material Accountant
|
|
2. COORDINATORS AND HEAD OF DEPARTMENTS
|
|
1.
|
Pr BENGONDO MESSANGA Charles
|
Coordinator of Dentistry Department
|
|
2.
|
Pr NTSAMA ESSOMBA Claudine
|
Coordinator of Pharmacy Department
|
|
3.
|
Pr ONGOLO ZOGO Pierre
|
Coordinator of Internist Department
|
|
4.
|
Pr ESSAME OYONO Jean Louis
|
Coordinator of Specialisation Cycle in Anatomy Pathology
Department
|
|
5.
|
Pr ZE MINKANDE Jacqueline
|
Coordinator of Specialisation Cycle in Anaesthesiology and
Reanimation Department
|
|
6.
|
Pr NGO NONGA Bernadette
|
Coordinator of Specialisation Cycle in General Surgery
Department
|
|
7.
|
Pr MBU ENOW Robinson
|
Coordinator of Specialisation Cycle in Gynaecology and Obstetrics
Department
|
|
8.
|
Pr NGANDEU Madeleine
|
Coordinator of Specialisation Cycle in Internal Medicine
Department
|
|
9.
|
Pr CHIABI Andreas
|
Coordinator of Specialisation Cycle in Paediatrics Department
|
|
10.
|
Pr GONSU Hortense
|
Coordinator of Specialisation Cycle in Clinical Biology
Department
|
|
11.
|
Pr NKO'O AMVENE Samuel
|
Coordinator of Specialisation Cycle in Radiology and Medical
Imagery Department
|
|
12.
|
Pr TAKOUGANG Innocent
|
Coordinator of Specialisation Cycle in Public Health
Department
|
|
HONORARY DIRECTORS OF CUSS
|
|
1.
|
Pr MONEKOSSO Gottlieb (1969-1978)
|
Internal Medicine/Neurology
|
|
2.
|
Pr EBEN MOUSSI Emmanuel (1978-1983)
|
Physiologic Science/Biochemistry; Pharmacology
|
|
3.
|
Pr NGU LIFANJI Jacob (1983-1985)
|
Internal Medicine/Nephrology
|
|
4.
|
Pr CARTERET Pierre (1985-1993)
|
Physiologic Sciences/Biochemistry; Physiology
|
|
HONORARY DEANS OF FMBS
|
|
1.
|
Pr SOSSO Maurice Aurélien (1993-1999)
|
Surgery and Specialties: General Surgery
|
|
2.
|
Pr NDUMBE Peter (1999-2006)
|
Haematology, Microbiology and Parasitology
|
|
3.
|
Pr TETANYE EKOE Bonaventure (2006-2012)
|
Paediatrics
|
|
4.
|
Pr EBANA MVOGO Côme (2012-2015)
|
Opthalmology/ORL
|
|
3. TEACHING STAFF
|
|
DEPARTMENT OF SURGERY AND SPECIALTIES
|
|
A. Professor Emeritus
|
|
1.
|
SOSSO Maurice Aurélien (CD)
|
General Surgery
|
|
2.
|
AFANE ELA Anatole
|
Anaesthesiology-Intensive care
|
|
3.
|
ANGWAFO III Fru
|
Surgery: Urology
|
|
4.
|
DJIENTCHEU Vincent de Paul
|
Surgery: Neurosurgery
|
|
5.
|
ESSOMBA Arthur
|
General Surgery
|
|
6.
|
NGOWE NGOWE Marcellin
|
General surgery
|
|
7.
|
ZE MINKANDE Jacqueline
|
Anaesthesiology- Intensive care
|
|
B. Associate Professors
|
|
1.
|
BEYIHA Gérard
|
Anaesthesiology- Intensive care
|
|
2.
|
ELOUNDOU NGAH J.
|
Surgery: Neurosurgery
|
|
3.
|
ESIENE Agnès
|
Anaesthesiology- Intensive care
|
|
4.
|
EYENGA Victor Claude
|
Surgery: Neurosurgery
|
|
5.
|
FARIKOU Ibrahima
|
Orthopaedic Surgery
|
|
6.
|
FOUDA Pierre
|
Surgery: Urology
|
|
7.
|
MOUAFO TAMBO Faustin
|
Paediatric Surgery
|
|
8.
|
NGO NONGA Bernadette
|
General Surgery
|
|
9.
|
ONDOBO ANDZE Gervais
|
Paediatric Surgery
|
|
10.
|
PISOH Christopher
|
General Surgery
|
|
C. Senior Lecturers
|
|
1.
|
AHANDA ASSIGA
|
General Surgery
|
|
2.
|
GUIFO Marc Leroy
|
General Surgery
|
|
3.
|
HANDY EONE Daniel
|
Orthopaedic Surgery
|
|
4.
|
OWONO ETOUNDI Paul
|
Anaesthesiology- Intensive care
|
|
5.
|
TSIAGADIGI Jean Gustave
|
Orthopaedic Surgery
|
|
D. Lecturers
|
|
1.
|
AMENGLE Albert Ludovic
|
Anaesthesiology- Intensive care
|
|
2.
|
BANG GUY Aristide
|
General surgery
|
|
3.
|
BENGONO BENGONO Roddy Stéphan
|
Anaesthesiology- Intensive care
|
|
4.
|
BWELE Georges
|
General surgery
|
|
5.
|
JEMEA Bonaventure
|
Anaesthesiology- Intensive care
|
|
6.
|
NGO YAMBEN Marie Ange
|
Orthopaedic Surgery
|
|
DEPARTMENT OF INTERNAL MEDICINE AND
SPECIALTIES
|
|
A. Professors Emeritus
|
|
1.
|
NJOYA OUDOU (CD)
|
Internal Medicine/Gastro-enterology
|
|
2.
|
AFANE ZE Emmanuel
|
Internal Medicine/Pulmonology
|
|
3.
|
BIWOLE SIDA Magloire
|
Internal Medicine/Hepato-Gastro-enterology
|
|
4.
|
KINGUE Samuel
|
Internal Medicine/Cardiology
|
|
5.
|
MBANYA Jean Claude
|
Internal Medicine/Endocrinology
|
|
6.
|
NDJITOYAP NDAM Elie Claude
|
Internal Medicine/Hepato-Gastro-enterology
|
|
7.
|
NDOM Paul
|
Internal Medicine/ Oncology
|
|
8.
|
NJAMNSHI Alfred K.
|
Internal Medicine/Neurology
|
|
9.
|
NOUEDOUI Christophe
|
Internal Medicine/ Endocrinology
|
|
10.
|
SINGWE Madeleine épse NGANDEU
|
Internal Medicine/Rhumatology
|
|
B. Associate Professors
|
|
1.
|
ANKOUANE ANDOULO
|
Internal Medicine/Hepato-Gastro-enterology.
|
|
2.
|
ASHUNTANTANG Gloria Enow
|
Internal Medicine/ Nephrology
|
|
3.
|
BISSEK Anne Cécile
|
Internal Medicine/Dermatology
|
|
4.
|
KAZE FOLEFACK François
|
Internal Medicine/Nephrology
|
|
5.
|
KUATE TEGUEU Calixte
|
Internal Medicine/Neurology
|
|
6.
|
MENANGA Alain Patrick
|
Internal Medicine/Cardiology
|
|
7.
|
NGOUNOU NOUBISSIE Marie ép. DOUALLA BIJA
|
Internal Medicine/Rheumatology
|
|
8.
|
SOBNGWI Eugène
|
Internal Medicine/Endocrinology
|
|
9.
|
YONE PEFURA
|
Internal Medicine/Pulmonology
|
|
C. Senior Lecturers
|
|
1.
|
ETOUNDI MBALLA Alain
|
Internal Medicine/Pulmonology
|
|
2.
|
FOUDA MENYE Hermine Danielle
|
Internal Medicine/Nephrology
|
|
3.
|
HAMADOU BA
|
Internal Medicine/Cardiology
|
|
4.
|
KAMGA OLEN Jean Pierre Olivier
|
Internal Medicine/Psychiatry
|
|
5.
|
KOUOTOU Emmanuel Armand
|
Internal Medicine/Dermatology
|
|
6.
|
KOWO Mathurin Pierre
|
Internal Medicine/Hepato- Gastro-enterology
|
|
7.
|
LOBE Emmanuel
|
Internal Medicine/Nephrology
|
|
8.
|
NDONGO AMOUGOU Sylvie
|
Internal Medicine/Cardiology
|
|
9.
|
NTONE ENYIME Félicien
|
Internal Medicine/Psychiatry
|
|
10.
|
ZE Jean Jacques
|
Internal Medicine/Pulmonology
|
|
D. Lecturers
|
|
1.
|
BOOMBHI Jérôme
|
Internal Medicine/Cardiology
|
|
2.
|
KUATE née MFEUKEU KWA Liliane Claudine
|
Internal Medicine/Cardiology
|
|
3.
|
NGANOU Chris Nadège
|
Internal Medicine/Cardiology
|
|
DEPARTMENT OF MEDICAL IMAGERY AND RADIOLOGY
|
|
1.
|
ZEH Odile Fernande (CD)
|
Radiology/Medical Imagery
|
|
A. Professors Emeritus
|
|
1.
|
GONSU Joseph
|
Radiology/Medical Imagery
|
|
2.
|
MOUELLE SONE
|
Radiotherapy
|
|
3.
|
NKO'O AMVENE Samuel
|
Radiology/Medical Imagery
|
|
B. Associate Professors
|
|
1.
|
ZEH Odile Fernande
|
Radiology/Medical Imagery
|
|
2.
|
GUEGANG GOUJOU. E.
|
Radiology/Neuroradiology
|
|
3.
|
MOIFO Boniface
|
Radiology/Medical Imagery
|
|
4.
|
ONGOLO ZOGO Pierre
|
Radiology/Medical Imagery
|
|
C. Lecturer
|
|
1.
|
MBEDE Maggy
|
Radiology/Medical Imagery
|
|
DEPARTMENT OF GYNAECOLOGY AND OBSTETRCS
|
|
A. Professors Emeritus
|
|
1.
|
KASIA Jean Marie (CD)
|
Gynaecology/Obstetrics
|
|
2.
|
BELLEY PRISO Eugène
|
Gynaecology/Obstetrics
|
|
3.
|
MBOUDOU Émile
|
Gynaecology/Obstetrics
|
|
4.
|
MBU ENOW Robinson
|
Gynaecology/Obstetrics
|
|
B. Associate Professors
|
|
1.
|
FOUMANE Pascal
|
Gynaecology/Obstetrics
|
|
2.
|
KEMFANG NGOWA J.D.
|
Gynaecology/Obstetrics
|
|
3.
|
NANA NJOTANG Philip
|
Gynaecology/Obstetrics
|
|
4.
|
NKWABONG Elie
|
Gynaecology/Obstetrics
|
|
5.
|
TEBEU Pierre Marie
|
Gynaecology/Obstetrics
|
|
C. Senior Lecturers
|
|
1.
|
BELINGA Etienne
|
Gynaecology/Obstetrics
|
|
2.
|
DOHBIT Julius SAMA
|
Gynaecology/Obstetrics
|
|
3.
|
FOUEDJIO Jeanne H.
|
Gynaecology/Obstetrics
|
|
4.
|
ESSIBEN Félix
|
Gynaecology/Obstetrics
|
|
5.
|
MVE KOH Valère Salomon
|
Gynaecology/Obstetrics
|
|
6.
|
NGO UM Esther Juliette épse MEKA
|
Gynaecology/Obstetrics
|
|
7.
|
NOA NDOUA Claude Cyrille
|
Gynaecology/Obstetrics
|
|
DEPARTMENT OF OPHTALMOLOGY, ENT AND
STOMATOLOGY
|
|
A. Professors Emeritus
|
|
1.
|
NDJOLO Alexis (CD)
|
ENT
|
|
2.
|
BELLA Assumpta Lucienne
|
Ophthalmology
|
|
3.
|
EBANA MVOGO Côme
|
Ophthalmology
|
|
4.
|
NJOCK Richard
|
ENT
|
|
B. Associate Professors
|
|
1.
|
DJOMOU François
|
ENT
|
|
3.
|
ELLONG Augustin
|
Ophthalmology
|
|
4.
|
ÉPÉE Émilienne
|
Ophthalmology
|
|
C. Senior Lecturers
|
|
1.
|
BILLONG Yannick
|
Ophthalmology
|
|
2.
|
DOHVOMA Andin Viola
|
Ophthalmology
|
|
3.
|
EBANA MVOGO Stève Robert
|
Ophthalmology
|
|
4.
|
KAGMENI Gilles
|
Ophthalmology
|
|
5.
|
KOKI Godefroy
|
Ophthalmology
|
|
6.
|
NGABA Olive
|
ENT
|
|
DEPARTMENT OF PAEDIATRICS
|
|
A. Professors Emeritus
|
|
1.
|
KOKI NDOMBO Paul (CD)
|
Paediatrics
|
|
2.
|
MONEBENIMP Francisca
|
Paediatrics
|
|
B. Associate Professors
|
|
1.
|
CHELO David
|
Paediatrics
|
|
2.
|
CHIABI Andreas
|
Paediatrics
|
|
3.
|
MAH Evelyn
|
Paediatrics
|
|
4.
|
NGUEFACK Séraphin
|
Paediatrics
|
|
C. Senior Lecturers
|
|
1.
|
KALLA Ginette Claude épse MBOPI KEOU
|
Paediatrics
|
|
2.
|
MBASSI AWA
|
Paediatrics
|
|
3.
|
NGO UM KINJEL Suzanne épse SAP
|
Paediatrics
|
|
4.
|
NGUEFACK épouse DONGMO Félicitée
|
Paediatrics
|
|
5.
|
NOUBI N. épouse KAMGAING M.
|
Paediatrics
|
|
6.
|
ONGOTSOYI Angèle H.
|
Paediatrics
|
|
DEPARTMENT OF MICROBIOLOGY, PARASITOLOGY, HEMATOLOGY
AND INFECTIOUS DISEASES
|
|
A. Professors Emeritus
|
|
1.
|
MBOPI KEOU François-Xavier (CD)
|
Bacteriology/Virology
|
|
2.
|
ADIOGO Dieudonné
|
Microbiology/Virology
|
|
3.
|
LUMA Henry
|
Bacteriology/Virology
|
|
4.
|
MBANYA Dora
|
Haematology
|
|
B. Associate Professors
|
|
1.
|
NKOA Thérèse
|
Microbiology /Haematology
|
|
2.
|
OKOMO ASSOUMOU Marie C.
|
Bacteriology/ Virology
|
|
3.
|
GONSU née KAMGA Hortense
|
Bacteriology
|
|
4.
|
TAYOU TAGNY Claude
|
Microbiology/Haematology
|
|
5.
|
TOUKAM Michel
|
Microbiology
|
|
C. Senior Lecturers
|
|
1.
|
CHETCHA CHEMEGNI Bernard
|
Microbiology/Haematology
|
|
2.
|
KINGE Thomson Njie
|
Infectious Diseases
|
|
3.
|
LYONGA Emilia ENJEMA
|
Medical Microbiology
|
|
D. Lecturers
|
|
1.
|
BEYELA Frédérique
|
Infectious Diseases
|
|
2.
|
NDOUMBA NKENGUE Annick épse MINTYA
|
Virology
|
|
3.
|
VOUNDI VOUNDI Esther
|
Virology
|
|
DEPARTMENT OF PUBLIC HEALTH
|
|
A. Professor Emeritus
|
|
1.
|
MONEBENIMP Francisca (CD)
|
Paediatrics
|
|
B. Associate Professors
|
|
1.
|
KAMGNO Joseph
|
Public Health/Epidemiology
|
|
2.
|
TAKOUGANG Innocent
|
Public Health
|
|
3.
|
TANYA née NGUTI K. A.
|
Nutrition
|
|
4.
|
ESSI Marie Josée
|
Public Health /Medical Anthropology
|
|
5.
|
NGUEFACK TSAGUE
|
Public Health /Biostatistics
|
|
C. Senior Lecturer
|
|
1.
|
BILLONG Serges Clotaire
|
Public Health
|
|
2.
|
BEDIANG Georges Wylfred
|
Medical Information Technology/ Public Health
|
|
3.
|
KEMBE ASSAH Félix
|
Epidemiology
|
|
4.
|
KWEDI JIPPE Anne Sylvie
|
Epidemiology
|
|
5.
|
NJOUMEMI ZAKARIAOU
|
Public Health /Health Economy
|
|
DEPARTMENTOF MORPHOLOGIC-ANATOMY PATHOLOGIC
SCIENCES
|
|
1.
|
SANDO Zacharie (CD)
|
Anatomy Pathology
|
|
A. Professors Emeritus
|
|
1.
|
ESSAME OYONO
|
Anatomy Pathology
|
|
2.
|
FEWOU Amadou
|
Anatomy Pathology
|
|
B. Associate Professors
|
|
1.
|
SANDO Zacharie
|
Anatomy Pathology
|
|
C. Senior Lecturers
|
|
1.
|
AKABA Désiré
|
Human Anatomy
|
|
2.
|
KABEYENE OKONO Angèle
|
Histology/Embryology
|
|
3.
|
MENDIMI NKODO Joseph
|
Anatomy Pathology
|
|
D. Lecturers
|
|
1.
|
NSEME Eric
|
Legal Medicine
|
|
DEPARTMENT OF BIOCHEMISTRY
|
|
1.
|
NDONGO EMBOLA épse TORIMIRO Judith
(CD)
|
Physiology/Molecular Biology
|
|
A. Professor Emeritus
|
|
1.
|
MBACHAM Wilfried
|
Biochemistry
|
|
B. Associate Professors
|
|
1.
|
NDONGO EMBOLA épse TORIMIRO Judith
|
Physiology/Molecular Biology
|
|
2.
|
PIEME Constant Anatole
|
Biochemistry
|
|
C. Senior Lecturers
|
|
1.
|
AMA MOOR Vicky Joceline
|
Clinical Biology/Biochemistry
|
|
D. Lecturers
|
|
1.
|
BONGHAM BERINYUI
|
Biochemistry
|
|
DEPARTMENT OF PHYSIOLOGY
|
|
A. Professor Emeritus
|
|
1.
|
ETOUNDI NGOA Laurent Serges (CD)
|
Physiology
|
|
B. Senior Lecturers
|
|
1.
|
ASSOMO NDEMBA Peguy Brice
|
Physiology
|
|
2.
|
AZABJI KENFACK Marcel
|
Physiology
|
|
C. Lecturers
|
|
3.
|
DZUDIE TAMDJA Anastase
|
Physiology
|
|
DEPARTMENT OF PHARMACOLOGY AND TRADITIONAL
MEDICINE
|
|
1.
|
NGONO MBALLA Rose ABONDO (CD)
|
African Pharmaco-therapeutics
|
|
A. Professors Emeritus
|
|
1.
|
NGADJUI CHALEU Bonaventure
|
Pharmacy/Phytochemistry
|
|
B. Senior Lecturers
|
|
1.
|
NGONO MBALLA Rose ABONDO
|
African Pharmaco-therapeutics
|
|
2.
|
NDIKUM Valentine
|
Pharmacology
|
|
DEPARTMENT OF BUCCAL SURGERY, MAXILLO-FACIAL AND
PARODONTOLOGY
|
|
A. Professors Emeritus
|
|
1.
|
BENGONDO MESSANGA Charles(CD)
|
Stomatology
|
|
B. Senior Lecturers
|
|
1.
|
MINDJA EKO David
|
ORL/ Maxillo-Facial Sugery
|
|
C. Lecturers
|
|
1.
|
BITHA BEYIDI Thècle Rose Claire
|
Maxillo Facial Surgery
|
|
2.
|
GAMGNE GUIADEM C.M
|
Dental Surgery
|
|
3.
|
NOKAM TAGUEMNE M.E.
|
Dental Surgery
|
|
DEPARTMENT OF PHARMACOTOXICOLOGY AND
PHARMACOKINETICS
|
|
1.
|
NGUIDJOE Evrard Marcel (CD)
|
Pharmacology
|
|
A. Associate Professors
|
|
1.
|
FOKUNANG Charles
|
Molecular Biology
|
|
2.
|
MPONDO MPONDO Emmanuel
|
Pharmaco-toxicology/ Pharmacokinetics
|
|
B. Senior Lecturers
|
|
1.
|
NGUIDJOE Evrard Marcel
|
Pharmacology
|
|
2.
|
TEMBE Estella épse FOKUNANG
|
Clinical Pharmacology
|
|
3.
|
TABI OMGBA
|
Pharmacy
|
|
DEPARTMENT OF PHARMACOGNOSY AND PHARMACEUTIC
CHEMISTRY
|
|
A. Associate Professors
|
|
1.
|
NTSAMA ESSOMBA Claudine (CD)
|
Pharmacognosy / Pharmaceutic Chemistry
|
|
2.
|
GUEDJE Nicole Marie
|
Ethnopharmacology/ Plant Biology
|
|
3.
|
NGAMENI Barthélémy
|
Phytochemistry/ Organic Chemistry
|
|
4.
|
NGOUPAYO Joseph
|
Phytochemistry/General Chemistry
|
|
DEPARTMENT OF GALENICAL PHARMACY AND PHARMACEUTIC
LEGISLATION
|
|
A. Associate Professors
|
|
1.
|
NNANGA NGA Emmanuel (CD)
|
Galenical Pharmacy
|
|
B. Lecturers
|
|
1.
|
MBOLE Jeanne Mauricette épse MVONDO M.
|
Quality Management, Quality Control of Health Products and
Food
|
|
2.
|
SOPPO LOBE Charlotte Vanessa
|
Quality Control of Medicines
|
Key: CD= Chief of Department
GALEN'S OATH
I swear, in the presence of the Masters of the Faculty and
my classmates:
To honour those who educated me in the precepts of my art
and to show them my gratitude by remaining faithful to their teaching.
To exercise, in the interest of public health, my
profession with consciousness and to respect not only the legislation in
effect, but also the rules of honour, probity and disinterestedness.
To never forget my responsibility and duties towards the
sick person and his human dignity; in no case, I shall consent to use my
knowledge and my status for corrupt mores and favour criminal acts.
That men grant me their esteem if I am faithful to my
promises. May I be covered with opprobrium and despised by my colleagues if I
don't.
ABSTRACT
BACKGROUND: Cardiovascular diseases account
for about 17 million deaths per year globally.Hypertension is responsible for
at least 45% of deaths due to heart disease. The number of people with
uncontrolled hypertension is increasing because of population growth and
ageing. A very high prevalence rate of hypertension of 29.7% was reported in
Cameroon. Hypertension requires long term management and follow-up. Adherence
to therapy is a key component of a successful management. Few studies have been
done in Cameroon regarding antihypertensive treatment adherence. This study was
therefore designed to assess the adherence status and associated factors to
antihypertensive therapy in hypertensive patients followed-up at Yaounde
General Hospital.
METHODS: This was a cross-sectional analytic
study conducted at the external consultation service of the cardiology unit of
the Yaounde General Hospital. This study was carried out over a period of seven
months (November 2017 - May 2018). Patients admitted into this study were
selected consecutively and those that met our inclusion criteria were selected
prior to interviewing. Two sitting blood pressure measurements were taken on
both arms with a pretested electronic sphygmomanometer. We assessed the
adherence level of the study population by using the validated Morisky 8-item
medication adherence scale. Patients with a score of 8 on the scale were
termedhighly adherent, medium adherers were those with a score of 6 to <8,
and those classified as lowadherers were those with a score of <6. Bivariate
and multivariate analyses were carried out to assess associations of each
independent variable with the dependent variable. Odds ratio and 95% confidence
interval were used to identify the presence and strength of association.
Statistical significance was considered at P-value < 0.05.
RESULTS:Of the 181 patients screened, 175
were retained for the study. Sex ratio of participants was 1.2 with male
predominance of 54.90%. The mean age was 60 years. Most participants (88.60%)
lived in urban areas and 51.43% had a non-liberal profession, the majority
(66.30%) lived as couples and 40.00% had a higher level of education. Trip
duration to the hospital was less than one hour for84.60% of participants. The
high socioeconomic status (60%) was highly representedin this study and 10.9%
of participants had a health insurance.The High Normal blood pressure group was
most represented (24.60%) and 57.70% had acontrolled BP. The most frequently
encountered comorbidity was heart failure(24.57%). Only 18.29% of participants
had a handicap. Calcium channel blockers were the most encountered monotherapy
(31.90%). The mean treatmentcost was 14543FCFA and most participants were in
the 10000-20000FCFAmonthly drug cost range. Poor adherence was observed in
32.60% of study participants. After multivariate analysis with logistic
regression, 9 variables were significantlyassociated with poor adherence: first
cycle secondary education (p=0.0209; odds ratio=4.6623), living
singly(p=0.0003; odds ratio=4.6623), tripduration of one hour or more (p=0.008;
odds ratio=7.3925), middle socioeconomic status (p=0.006; odds ratio=2.6814),
uncontrolled blood pressure status(p<0.0001; odds ratio=5.5704),presence of
handicap (p=0.0117; odds ratio=4.1222), monotherapy (p=0.0295; odds
ratio=2.0721), presence of side effects (p<0.0001; odds ratio=11.5143), and
taking medication inthe evening (p=0.0399; odds ratio=2.5452).Of the 74
patients with uncontrolled BP, 86.49% had poor adherence. Only 54.30% of
participants were knowledgeable about hypertension.
CONCLUSION: 9 predictive factors of poor
adherence were identified: first cycle secondary education, living singly,
tripduration of one hour or more, middle socioeconomic status, uncontrolled BP
status,presence of handicap, monotherapy, presence of side effects, and taking
medications inthe evening. Addressing these factors could help health care
providers better foster drug adherence.
Keywords: Adherence, antihypertensive, Morisky,
Yaounde
RESUME
CONTEXTE: Les maladies cardiovasculaires
causent environ 17 millions de décès par an dans le monde.
L'hypertension est responsable d'au moins 45% des décès dus
à une maladie cardiaque. Le nombre de personnes souffrant d'hypertension
incontrôlée augmente en raison de la croissance
démographique et du vieillissement. Un taux très
élevé de prévalence de l'hypertension de 29,7% a
été signalé au Cameroun. L'hypertension nécessite
une prise en charge à long terme et un suivi. L'observance aux
traitements est un élément clé d'une prise en charge
réussie. Peu d'études ont été
réalisées au Cameroun concernant l'observance aux traitements
antihypertenseurs. Cette étude a donc été conçue
pour évaluer le niveau d'observance et les facteurs associés aux
traitements antihypertenseurs chez des patients hypertendus suivis à
l'Hôpital général de Yaoundé.
METHODES: C'est une étude analytique
et transversale et réalisée au service de consultations externe
de l'unité de cardiologie de l'Hôpital Général de
Yaoundé. Elle a été menée sur une période de
sept mois (novembre 2017 - mai 2018). Les patients admis dans cette
étude ont été sélectionnés
consécutivement et ceux qui répondaient à nos
critères d'inclusion ont été sélectionnés
avant d'être interviewés. Deux mesures de la pression
artérielle étant assis, ont été prises sur les deux
bras avec un sphygmomanomètre électronique
prétesté. Nous avons évalué le niveau d'observance
de la population étudiée en utilisant l'échelle
d'observance des médicaments en 8 points de Morisky. Les patients avec
un score de 8 sur l'échelle ont été
considérés comme hautement observant, les observant moyens ont
été ceux avec un score de 6 à <8, et ceux
classés comme faiblesobservant étaient ceux avec un score <6.
Des analyses bi-variées et multivariées ont été
réalisées pour évaluer les associations de chaque variable
indépendante avec la variable dépendante. L'Odds ratio et
intervalle de confiance à 95% ont été utilisés pour
identifier la présence et la force de l'association. La signification
statistique a été considérée à la valeur P
<0,05.
RÉSULTATS:Après avoir
identifié 181 patients, 175 ont été retenus pour
l'étude. Le sex-ratio des participants était de 1,2 avec une
prédominance masculine de 54,90%. L'âge moyen était de 60
ans. La plupart des participants (88,60%) vivaient en milieu urbain et 51,43%
avaient une profession non libérale, la majorité (66,30%) vivait
en couple et 40,00% avaient un niveau de scolarité plus
élevé. La durée du trajet à l'hôpital
était de moins d'une heure pour 84,60% des participants. Le statut
socioéconomique élevé (60%) était largement
représenté dans cette étude et 10,9% des participants
avaient une assurance santé. Le groupe Haut Normal de pression
artérielle était le plus représenté (24,60%) et
57,70% avaient une pression artérielle contrôlée. La
comorbidité la plus fréquente était l'insuffisance
cardiaque (24,57%). Seulement 18,29% des participants avaient un handicap. Les
inhibiteurs calciques ont été les monothérapies les plus
rencontrées (31,90%). Le coût moyen du traitement était de
14543FCFA et la plupart des participants se situaient dans la fourchette des
coûts mensuels de 10000-20000FCFA. La mauvaise observance a
été retrouvée chez 32,6% des participants. Après
analyse multivariée avec régression logistique, 9 variables
étaient significativement associées à une mauvaise
observance: enseignement secondaire de premier cycle(p=0.0209; odds
ratio=4.6623), vie seule(p=0.0003; odds ratio=4.6623), durée du trajet
d'une heure ou plus(p=0.008; odds ratio=7.3925), statut socioéconomique
moyen(p=0.006; odds ratio=2.6814), état de PA
incontrôlé(p<0.0001; odds ratio=5.5704), présence d'un
handicap(p=0.0117; odds ratio=4.1222), monothérapie(p=0.0295; odds
ratio=2.0721), présence d'effets secondaires(p<0.0001; odds
ratio=11.5143) et prise médicamenteuse le soir(p=0.0399; odds
ratio=2.5452). Sur les 74 patients avec une pression artérielle non
contrôlée, 86,49% avaient une mauvaise observance. Seulement
54,30% des participants connaissaient l'hypertension.
CONCLUSION: 9 facteurs prédictifs de
mauvaise observance ont été identifiés: enseignement
secondaire de premier cycle, vie seule, durée de voyage d'une heure ou
plus, statut socioéconomique moyen, état de PA
incontrôlé, présence d'un handicap, monothérapie,
présence d'effets secondaires et prise de médicaments le soir.
S'attaquer à ces facteurs pourrait aider les fournisseurs de soins de
santé à mieux favoriser l'observance aux médicaments
antihypertenseurs.
Mots-clés: Observance,
antihypertenseur, Morisky, Yaoundé
LIST OF FIGURES
FIGURE 1: CEREBROVASCULAR DISEASE MORTALITY
RATES
1
FIGURE 2: AGE-STANDARDIZED PREVALENCE OF RAISED
BLOOD PRESSURE IN ADULTS AGED 25+ YEARS
7
FIGURE 3: DISTRIBUTION OF THE WORLD'S POPULATION BY
AGE AND SEX, 2015
9
FIGURE 4: PROJECTED GLOBAL DEATHS FOR SELECTED
CAUSES, 2004-2030
9
FIGURE 5: ADDITIVE EFFECT OF HYPERTENSINOGENIC
FACTORS ON HEREDITARY SYSTOLIC AND DIASTOLIC BLOOD PRESSURE
11
FIGURE 6: SITES OF ACTION OF DRUGS AFFECTING THE
RENIN-ANGIOTENSIN SYSTEM
24
FIGURE 7: DUTCH LIPID CLINIC CRITERIA
54
FIGURE 8: PARTICIPANT FLOW CHART
60
FIGURE 9: DISTRIBUTION ACCORDING TO SOCIOECONOMIC
STATUS
63
FIGURE 10: DISTRIBUTION ACCORDING TO POSSESSION OF
HEALTH INSURANCE
63
FIGURE 11: BLOOD PRESSURE DISTRIBUTION OF THE STUDY
POPULATION ON ENROLMENT
64
FIGURE 12: BLOOD PRESSURE STATUS DISTRIBUTION OF
THE STUDY POPULATION
65
FIGURE 13: DISTRIBUTION OF COMORBIDITIES OF THE
STUDY POPULATION
66
FIGURE 14: DISTRIBUTION ACCORDING TO TYPE OF
HANDICAP
67
FIGURE 15: DISTRIBUTION OF ADHERENCE LEVELS
71
FIGURE 16: DISTRIBUTION ACCORDING TO LEVEL
KNOWLEDGE ON HYPERTENSION
73
LIST OF TABLES
TABLE I: BLOOD PRESSURE MEASUREMENT
1
TABLE II: BLOOD PRESSURE THRESHOLDS FOR DEFINITION
OF HYPERTENSION WITH DIFFERENT TYPES OF MEASUREMENT
17
TABLE III: PHYSICAL EXAMINATION FOR SECONDARY
HYPERTENSION, ORGAN DAMAGE AND VISCERAL OBESITY
18
TABLE IV: LABORATORY INVESTIGATIONS
20
TABLE V: CLASSES AND SUBCLASSES OF ANTIHYPERTENSIVE
MEDICATIONS WITH COMMON EXAMPLES
23
TABLE VI: THE 8-ITEM MEDICATION ADHERENCE SCALE
57
TABLE VII: CUT-OFFS FOR THE 8-ITEM MEDICATION
ADHERENCE SCALE
58
TABLE VIII: SOCIODEMOGRAPHIC CHARACTERISTICS OF THE
STUDY POPULATION
62
TABLE IX: DISTRIBUTION ACCORDING TO CLASS OF
ANTIHYPERTENSIVE USED BY THE STUDY POPULATION ON ENROLMENT
68
TABLE X: DISTRIBUTION OF THERAPEUTIC VARIABLES
70
TABLE XI: DISTRIBUTION OF ADHERENCE PROFILES
71
TABLE XII: DISTRIBUTION ACCORDING TO BLOOD PRESSURE
STATUS AND GOOD ADHERENCE
72
LIST OF
ABBREVIATIONS/ACRONYMS/SYMBOLS
|
ACE
|
: Angiotensin-converting enzyme
|
|
ACEI
|
: Angiotensin-converting enzyme inhibitor
|
|
AHT
|
: Antihypertensive therapy
|
|
ARA
|
: Angiotensin receptor antagonist
|
|
BMI
|
: Body mass index
|
|
BP
|
: Blood pressure
|
|
CCB
|
: Calcium channel blocker
|
|
CI95
|
: 95% Confidence interval
|
|
DALY
|
: Disability-Adjusted Life Year
|
|
DRI
|
: Direct renin inhibitor
|
|
DBP
|
: Diastolic blood pressure
|
|
HBP
|
: High Blood Pressure
|
|
HDL
|
: High density lipoprotein
|
|
hsCRP
|
: High sensitivity C reactive protein
|
|
I.V.
|
: Intravenous
|
|
LDL
|
: Low density lipoprotein
|
|
MISS
|
: Medical Interview Satisfaction Scale
|
|
MMAS-8
|
: Eight-Item Morisky Medication Adherence Scale
|
|
NSAID
|
: Non-steroidal anti-inflammatory drug
|
|
OR
|
: Odds ratio
|
|
PA
|
: Primary aldosteronism
|
|
RAS
|
:Renin-angiotensin system
|
|
SBP
|
: Systolic blood pressure
|
|
SVR
|
: Systemic vascular resistance
|
|
TDM
|
: Therapeutic Drug Monitoring
|
|
UK
|
: United Kingdom
|
|
WHO
|
: World Health Organization
|
|
YGH
|
: Yaounde General Hospital
|
CHAPTER I: INTRODUCTION
I.1 BACKGROUND AND
RATIONALE
According to the World Health Organization (WHO),
cardiovascular diseases account for about 17 million deaths per year globally
i.e. nearly one third of the total[1].Of these cardiovascular
diseases, hypertension accounts for 9.4 million deaths worldwide and7.0% of
global disability adjusted life-years (DALY) in
2010[2].Hypertension is a serious medical condition and a key
public health problem.It has been defined as the level of blood pressure above
which intervention has been shown to reduce the associatedcardiovascular
risk[3].Hypertension is responsible for at least 45% of deaths
due to heart disease, and 51% of deaths due to stroke[1]. In
2008, approximately 40% of adults aged 25 and over had been diagnosed with
hypertension worldwide[4].The number of people with
uncontrolled hypertension increased from 605 million in 1980, to 978 million in
2008, because of population growth and ageing[5].Systolic
blood pressure (SBP) is currently highest in low-income and middle-income
countries[1,5,6];the prevalence of hypertension is highest in
the African continent at 46% of adults aged 25 and over, while the lowest
prevalence at 35% is found in the Americas[1]. In developing
countries, its morbidity andmortality are increasing due tosedentary life and
changes in lifestyle[7]. In 2015, Kingue et al. reported a
very high prevalence rate of hypertension (29.7%) in Cameroon, with the
tendency of a steady rise towards a super epidemic in the next 20 years to
come[8].Kamadjeu et al. reported in a 2003 population survey
that only 23% of all hypertensive patients were aware of their status, 10.8%
were taking antihypertensive medication and 2% were
controlled[9]. These findings suggest that medication
nonadherence might be responsible for the prevalence of high BP levels in
Cameroon. With this in mind, effective strategies have to be developed in order
to foster adherence to antihypertensive treatments by patients. The latter must
be encouraged to participate in medical decisions by actively getting involved
in the selection, adjustmentof drug treatment and in changes in lifestyle in
orderto maximize the usefulness of the
therapeuticregimen[10].
The adverse health effects of hypertensionare compounded
because manyaffected people also have other health risk factorsthat increase
the odds of heart attack,stroke and kidney failure[1]. These
risk factorsinclude tobacco use, obesity, high cholesteroland diabetesmellitus.
In 2008, 1 billion people weresmokers and the global prevalence of obesity
increased by about two-fold since 1980[1]. The global
prevalenceof high cholesterol was 39% and prevalenceof diabetes was 10% in
adults above 25 years[4].Populations around the world are
rapidly ageing and prevalence of hypertensionincreases with
age[11].
Treatment of hypertension involves both non-pharmacological
and pharmacological interventions to reduce blood pressure, as well as
assessment and treatmentof any other cardiovascular risk
factors[3].Adopting a healthy lifestyle is beneficial for all
individuals, and any patient with raised blood pressure should be encouraged to
make lifestyle changes that will reduce theircardiovascular risk. Depending on
treatment guidelines, different drug regimens may be used with differing
pharmacological actions. Historically, thiazide diuretics and beta blockers
have been the mainstay of drug therapy for hypertension, but calcium channel
blockers, angiotensin-converting enzyme inhibitors, antagonists of angiotensin
II receptors, and alpha blockers are now also widely
used[3].
Hypertension requires long term management and follow-up.
Adherence to therapy is a key component of a successful management. Adherence
to a medication regimen is generally defined as the extent to which patients
take medications as prescribed by their health care
providers[10].Both medications andlifestyle changes are
prescribed to hypertensive patients with the expectation that they will be
adherent[1,12].However, the problem of non-adherence tomedical
treatment remains a challenge for the medicalprofessions asmany patients fail
to adhere totreatment recommendations resulting inpoor health outcomes,lower
quality of life and increased health care costs[7,13].Poor
adherence to anti-hypertensive therapy is one of the biggest hindrances in
therapeutic control of high blood pressure[14].It also
compromises the efforts of healthcare systems, policy makers and health care
professionalsto improve the health of populations. Failure to adherecauses
medical and psychological complications of thedisease, reduces patients'
quality of life, wastes healthcare resources and erodes public confidence in
healthsystems[15].
Few studies have been done in Cameroon regarding
antihypertensive treatment adherence and the few that have been carried out
portray low levels of therapeutic adherence.Mbouemboue et al. found that
adherence to antihypertensive drug treatment is poor in their study population
in Garoua with an adherence rate of 12.9%[16].In a survey
conducted in the Buea Regional Hospital, it was noted that 94% of patients were
aware of the necessary measures to control their blood pressure, although 54.5%
affirmed having difficulties in respecting recommended dietary and other
lifestyle measures because they were too constraining[17].
Tufon et al. however reported a high overall level ofadherence of patients to
antihypertensive treatment (80.0%) in a rural setting (Mankon sub divisional
health centre)[18].Essomba et al. reported that 26.2% of their
study population in Douala had good adherence to antihypertensive
treatment[19]. Akoko et al. found a slightly greater adherence
rate of 49.3% among adult patients in the Bamenda Health
District[20].
Poor adherence to antihypertensive therapy is usually
associated with adverse clinical outcome of the disease andwastage of limited
health care resources[10,15,21]. The intention of addressing
adherence issues is to contribute in achieving the third sustainable goals
which seeks to «ensure healthy lives and promote wellbeing for all at all
ages»; especially target 24 which seeks to reduce by 2030, one third of
premature mortality from non-communicable diseases through prevention and
treatment and promote mental health and well-being[22].
The choice to undertake this study in the Yaounde General
Hospital was because it is a first category referral hospital with a
well-equipped cardiology service where many patients with various
cardiovascular diseases especially hypertensive patients are regularly followed
by cardiologists.
In Cameroon, there is a paucity of research regarding
adherence rates and their correlates in urban settings.This study was therefore
designed toassess the adherence statusand associated factors to
antihypertensive therapy in hypertensive patients followed-up at the Cardiology
Unit of the Yaounde General Hospital.
I.2 RESEARCH QUESTION
What is the level of adherence to antihypertensive treatment
and associated factors in hypertensive patients followed up at the Yaounde
General Hospital?
I.3 RESEARCH HYPOTHESIS
Adherence to antihypertensive treatments by patients followed
up at the Yaounde GeneralHospital is low and may beassociated with certain
factors.
I.4 OBJECTIVES
v GENERAL OBJECTIVE
To assess the adherence level and its associated factors to
antihypertensive therapy among adult hypertensive patients followed-up at the
Yaounde General Hospital.
v SPECIFIC OBJECTIVES
1. Document the sociodemographic and socioeconomic
characteristics of the study population.
2. Describe the clinical andtherapeutic characteristics of the
study population.
3. Assess their adherence to antihypertensive treatment using
a standard validated questionnaire.
4. Determine factors associated with antihypertensive poor
treatmentadherence.
5. Evaluate the association between BP and adherence data.
CHAPTER II: LITERATURE
REVIEW
I. GENERAL OVERVIEW
A. DEFINITION OF TERMS
· Adherence (to a medication
regimen): The World Health Organization (WHO) defines adherence as ``the extent
to which a person's behaviour taking medication, following a diet, and/or
executing life style changes corresponds with agreed recommendations from a
health care provider''[23].
· Disability-Adjusted Life Year
(DALY):Measure of years of life lost from deaths which occur before
some theoretically achievable age (e.g., international reports use 80 years for
men and 82.5 years for women) and attributing this loss to death rates. DALYs
for a disease or health condition are calculated as the sum of the Years of
Life Lost due to premature mortality in the population and the Years Lost due
to Disability for people living with the health condition or its
consequences[24].
· Compliance: Term suggesting that a
patient is passively following the doctor's orders and that the treatment plan
is not based on a therapeutic alliance or contract established between the
patient and the physician[10].
· Hypertension:Systolic blood pressure
equal to or above 140 mm Hg and/or diastolic blood pressure equal to or above
90 mm Hg[1].
B. EPIDEMIOLOGY OF HYPERTENSION
In 2010, the three leading risk factors for global disease
burden were high bloodpressure (7.0% of global DALYs), tobacco smoking
includingsecond-hand smoke (6.3%), and alcohol use (5.5%)[2].
Hypertension alone accounts for 9.4 million deaths
worldwide[1].Dietaryrisk factors and physical inactivity
collectively accounted for 10.0% of globalDALYs in 2010, with the most
prominent dietary risks being diets low in fruits and those high
insodium[2].Hypertension is responsible for at least 45% of
deaths due toheart disease, and 51% of deaths due
tostroke[1].Figure 1 shows the total stroke mortality rate in
the world.Globally, the overall prevalence of raised blood pressure in adults
aged 25 and over was around 40% in 2008[4].Figure 2 shows the
global age-standardized prevalence of raised blood pressure in adults aged 25+
years.The proportion of the world's population with high blood pressure, or
uncontrolled hypertension, fell modestly between 1980 and 2008. However,
because of population growth and ageing, the number of people with hypertension
rose from 600 million in 1980 to nearly 1 billion in 2008[4].
Still in 2008, the prevalence of raised blood pressure was highest in the
African continent, where it was 46% for both sexes
combined[4].
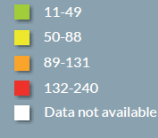
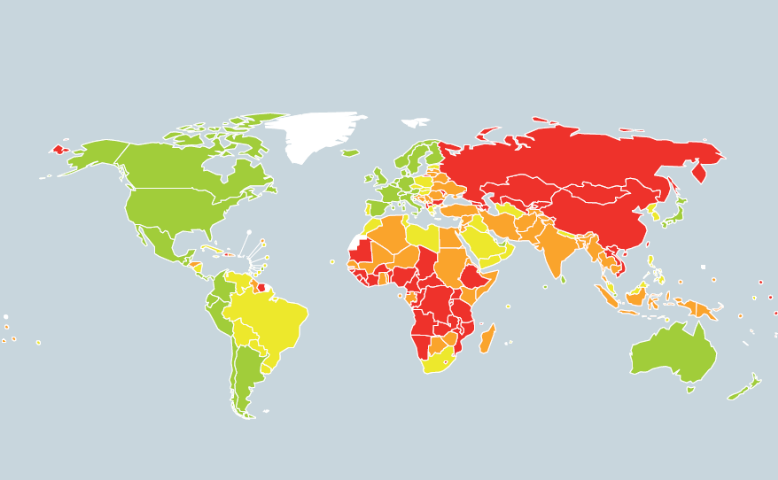
Figure 1: Cerebrovascular disease mortality
rates[1]

Figure 2: Age-standardized
prevalence of raised blood pressure in adults aged 25+ years[4]
The lowest prevalence of raised blood pressure was in the WHO
Region of theAmericas, with 35% for both sexes[4]. In all WHO
regions, men have slightly higher prevalence of raised blood pressure than
women, but this difference was only statistically significant in the American
and European continents[4].Across the income groups of
countries, the prevalence of raised blood pressure was consistently high in low
and lower-middle income countries while upper-middle-income countries all had
rates of around 40%for both sexes. The prevalence in high-income countries was
lower, at 35% for both sexes[4].Not only is hypertension more
prevalent in low- and middle-income countries, there are also more people
affected because more people live in those countries than in high-income
countries[1,5].Further, because of weak health systems, the
number of people with hypertension who are undiagnosed, untreated and
uncontrolled are also higher in low- and middle-income countries compared to
high-income countries. The increasing prevalence of hypertension is attributed
to population growth, ageing and behavioural risk
factors[1,11].Figure 3 shows the 2015 distribution of the
world's population by age and sex.
The adverse health consequences of hypertensionare compounded
because many peopleaffected also have other health risk factorsthat increase
the odds of heart attack,stroke and kidney failure. These risk factorsinclude
tobacco use, obesity, high cholesteroland
diabetesmellitus[1].In 2008, 1 billion people weresmokers and
the global prevalence of obesity has nearly doubled since
1980[1]. The global prevalenceof high cholesterol was 39% and
prevalenceof diabetes was 10% in adults over 25years[4].
Tobacco use, unhealthy diet, harmfuluse of alcohol and physical inactivity are
alsothe main behavioural risk factors of all majornoncommunicable diseases,
i.e. cardiovasculardisease, diabetes, chronic respiratory disease and cancer.If
appropriate action[1] is not taken, deaths dueto
cardiovascular disease are projected to rise further
[25].Figure 4 shows the projected global deaths for selected
causes for the 2004-2030 timeframe.
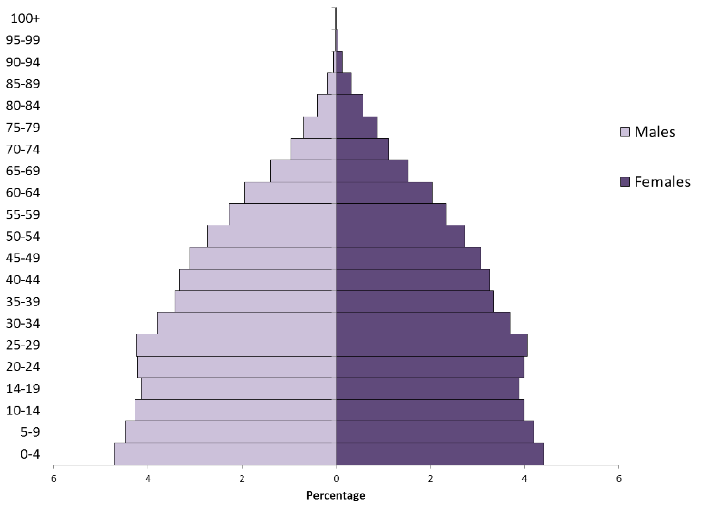
Figure 3: Distribution of the
world's population by age and sex, 2015[11]
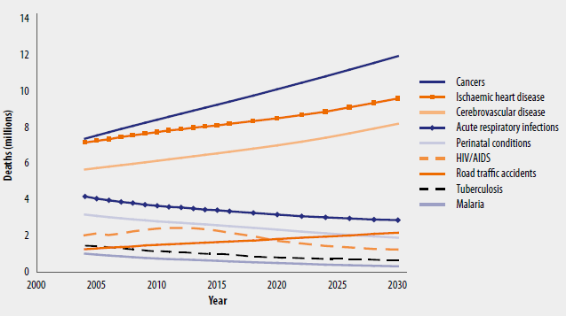
Figure 4: Projected global
deaths for selected causes, 2004-2030[25]
Between 1994 and 2003, blood pressure levels havedeteriorated
over time in rural and urban Cameroonian menand women with the prevalence of
hypertension increasing by twofold to fivefold[26].This has
beenattributed to the rapid urbanization associated with thehigh rates of
obesity, physical inactivity, diabetes,increased salt consumption, and tobacco
use[27].In 2011, Dzudie A et al. reported a prevalence rate
for hypertension of up to 47.5% in self-selectedurban dwellers in
Cameroon[28].In a more recent nationwide study, Kingue et al.
found a prevalence rate of 29.7% in urban areas of Cameroon;indicating
asteadyrise in the trend of hypertension toward a super epidemic in 20 years to
come[8].
C. CAUSES OF HYPERTENSION
In the majority of cases, high BP is termedprimary or
essentialhypertensionand isprobably multifactorial in origin, with genotype, as
well asexternal factors such as diet and body-weight, playing arole.
Hypertension may also be associated with surgery[29]or
pregnancy[30] and is prevalent in
diabetics[31]. In a limitednumber of cases hypertension is
secondaryto some othercondition, such as renal disease, Cushing's
syndrome,phaeochromocytoma, or to the adverse effects of drugs suchas
oestrogens, and such causes may be suspected particularlyin resistant or
malignant hypertension[32].
1. Primary or essential
hypertension[1,33,34]
Although it has frequently been indicated that the causes
ofessential hypertension are unknown, this is only partially true because
little information is available on genetic variationsor genes that are
over-expressed or under-expressed as well asthe intermediary phenotypes that
they regulate to cause hypertension.Variation in BP that is genetically
determined is called «inherited BP,»although the genes which cause BP
to vary are not known; it is known from familystudies that inherited BP can
range from low normal BP tosevere hypertension. Factors that increase BP, (such
as obesity, insulin resistance, high alcohol intake, high salt intake (in
salt-sensitive patients), ageing and perhapssedentary lifestyle, stress, low
potassium intake, and low calcium intake) are called «hypertensinogenic
factors.» Some of these factors have inherited,behavioural, and
environmental components. Inherited BPcould be considered core BP, whereas
hypertensinogenicfactors cause BP to increase above the range of inherited BPs.
Figure 5 illustrates the additive effect of hypertensinogenic factors on
hereditary systolic and diastolic BP. It shows that patients with normalor high
normal inherited BP become hypertensive stage 1 whenBP is increased by a
hypertensinogenic factor. In patients withinherited hypertension in stages 1 to
3, their hypertensionbecomes more severe when hypertensinogenic factors
areadded.
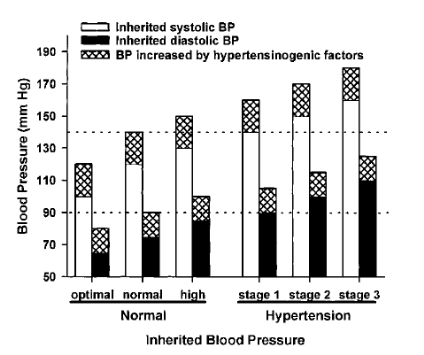
Figure 5: Additive effect
of hypertensinogenic factors (hatched areas) on hereditary systolic (white
areas) and diastolic blood pressure (black areas)[33]
2. Secondary hypertension[32,35,36]
Hypertension related to a specific aetiology is termed
secondaryhypertension,markedly differing from essential hypertension, ofwhich
the aetiology cannot be clearly identified. Secondary hypertension is often
resistant hypertension,for which a target blood pressure is difficult to
achieve bystandard treatment. However, BP can be effectivelyreduced by
identifying its aetiology and treating the condition.
Frequent etiological factors for secondary hypertension
includerenal parenchymal hypertension, primary aldosteronism (PA),
renovascularhypertension and sleep apnea syndrome. As other etiological factors
for secondary hypertension, the following conditions have been reported in
endocrine hypertension: pheochromocytomaand Cushing's syndrome which are
related to an excessiveproduction of catecholamines and cortisol, respectively.
Hypo-/hyperthyroidism, hyperparathyroidism and acromegaly are alsoetiologically
involved in hypertension. In vascular hypertension, angiitissyndrome, such as
aortitis syndrome, polyarteritis nodosa (PN)and systemic scleroderma, aortic
coarctation and aortic insufficiencyhave been reported. Compression of the
rostral ventrolateral medullaby brainstem blood vessels causes hypertension
through hyperactivityof the sympathetic nerves. Furthermore, hypertension is
also observedin patients with brain tumours or cerebrovascular disease. In
addition,drug-induced hypertension has been reported (by drugs such as NSAIDs,
oral contraceptive, liquorice, sympathomimetics, glucocorticoids,
cyclosporine, tacrolimus, erythropoietin, tricyclic/tetracyclic
antidepressants, monoamine oxygenase inhibitors, Anti-VEGF antibody
preparations).
It has been recognized that secondary hypertension accounts
for about 10% of hypertensive patients. According to several studies, PA
accounts for approximately 5-10% of hypertensive patients, and it is the most
frequent in endocrine hypertension.
Generally, the presence of severe or resistant hypertension,
juvenile hypertension and the rapid onset of hypertension suggest the
possibility of secondary hypertension. In such hypertensive patients, a close
inquiry on medical history, medical examination and adequate examinations must
be performed, considering the possibility of secondary hypertension. The
possibility of secondary hypertension should be considered in the diagnosis and
treatment of all hypertensive patients. It is important to conduct appropriate
examinations without overlooking findings of secondary hypertension.
D. THE SYMPTOMS OF HIGH BP AND ITS
COMPLICATIONS[1,37,38]
There is a common misconceptionthat people with
hypertensionalwaysexperience symptoms, but the reality isthat mosthypertensive
people have nosymptoms at all. The condition is a silent killer. Therefore it
is important for everybody to know their blood pressure reading.
Sometimes hypertensioncauses symptoms such as headache,
shortnessof breath, dizziness, chest pain, palpitationsof the heart and nose
bleeds. It canbe dangerous to ignore such symptoms,but neither can they be
relied upon to signifyhypertension.
Left untreated, high BP can have damaging effects. Theprimary
way it causes harm is by increasing the workload of the heart and
arteries,which causes damage to the circulatory system over time. Also, high BP
can cause the heart to enlarge because it has to work harderto supply the blood
the body needs. It is also a contributing factor toatherosclerosis, in which
the walls of the arteries become stiff and brittle as fattydeposits build up
inside them. Other conditions caused by hypertension include coronary heart
disease, heart failure, heartattack, stroke, kidney damage, angina (chest pain
related to heart disease), peripheralartery disease, and other serious
conditions (aneurysms, cognitive changes, eye damage). In fact, people with BP
over 140/90 are far more likely to havethese dangerous conditions thus
hypertension is a serious warning sign that significant lifestyle changes have
to be adopted.
E. DIAGNOSTIC EVALUATION
Current options for BP measuring devices include mercury
sphygmomanometers, aneroid manometers, semiautomatic devices and fully
automatic electronic devices. Validated and affordable electronic BP measuring
devices, that have the option to select manual readings, appear to be the
preferred option for lowresource settings according to
WHO[39].Semi-automatic devices enable manual readingsto be
taken when batteries run down,a common problem in resource-constrainedsettings.
Given that mercury is toxic,it is recommended that mercury devices bephased out
in favour of electronic devices[39].Aneroid devices should be
considered only if calibrated at regular intervals (every 6 months for example)
and users should be trained and assessed in measuring BP using such
devices[1,39].
Diagnostic procedures aim at: 1) establishing blood
pressurelevels; 2) identifying secondary causes of hypertension;3) evaluating
the overall cardiovascular risk bysearching for other risk factors, target
organ damageand concomitant diseases or accompanying clinicalconditions.The
diagnostic procedures comprise[40]:
- repeated blood pressure measurements
- medical history
- physical examination
- laboratory and instrumental investigations.
Some ofthese should be considered part of the routine
approachin all subjects with high BP; some arerecommended and may be used
extensively in thedeveloped health systems; some are indicatedonly when
suggested by the basic examination or theclinical course of the
patient[40].
1. Blood pressure measurement[1,40-42]
Blood pressure is characterized by large spontaneousvariations
both during the day and between days, monthsand seasons.Therefore the diagnosis
of hypertension should be based on multiple BP measurements, taken on separate
occasions over a period of time. If BP is only slightly elevated, repeated
measurements should be obtained over a period of several months to define the
patients ``usual'' BP as accurately as possible. On the other hand, if the
patient has a more marked BP elevation, evidence of hypertension-related organ
damage or a high or very high cardiovascular risk profile, repeated
measurements should be obtained over shorter periods of time (weeks or days).
In general, the diagnosis of hypertension should be based on at least 2 blood
pressure measurements per visit and at least 2 to 3 visits, although in
particularly severe cases the diagnosis can be based on measurements taken at a
single visit. Blood pressures can be measured by the doctor or the nurse in the
office or in the clinic (office or clinic blood pressure), by the patient or a
relative at home, or automatically over 24 h. Based on specific recommendations
of the European Society of Hypertension[40], these procedures
can be summarized as follows:
1.1 Office or clinic blood pressure
BP can be measured by a mercury sphygmomanometer the various
parts of which (rubber tubes, valves, quantity of mercury, etc.) should be kept
in proper working order. Other non-invasive devices (auscultatory or
oscillometric semiautomatic devices) can also be used and will indeed become
increasingly important because of the progressive banning of the medical use of
mercury[39]. However, these devices should be validated
according to standardized protocols[43], and their accuracy
shouldbe checked periodically by comparison with mercurysphygmomanometric
values. Table I shows the instructions for correctoffice BP measurements.
1.2 Ambulatory blood
pressure
Several devices (mostly oscillometric) are available
forautomatic BP measurements in patients allowed to conduct a near normal life.
They provide information on 24-hour average BP as well as on mean values over
more restricted periods such as the day, night or morning. This information
should not be regarded as a substitute for information derived from
conventional BP measurements. Studies have shown that ambulatory BP : 1)
correlates with hypertension-related organ damage and it changes by treatment
more closely than does office blood pressure, 2) has a relationship with
cardiovascular events that is steeper than that observed for clinic BP, with a
prediction of cardiovascular risk greater than the prediction provided by
office BP values in populations of untreated and treated
hypertensives[44-46] and 3) measures more accurately than
clinic BP the extent of BP reduction induced by treatment, because of a higher
reproducibility over time and an absent or negligible ``white
coat''[47] and placebo effect[48].
Table I: Blood pressure (BP)
measurement[40]
|
When measuring BP, care should be taken to:
|
|
1
|
Allow the patients to sit for several minutes in aquiet room
before beginning BP measurements
|
|
2
|
Take at least two measurements spaced by1-2 minutes, and
additional measurements if thefirst two are quite different
|
|
3
|
Use a standard bladder (12-13 cm long and 35 cmwide) but have a
larger and a smaller bladderavailable for fat and thin arms, respectively.
Usethe smaller bladder in children
|
|
4
|
Have the cuff at the heart level, whatever theposition of the
patient
|
|
5
|
Use phase I and V (disappearance) Korotkoffsounds to identify
systolic and diastolic BP,respectively
|
|
6
|
Measure BP in both arms at first visit to detectpossible
differences due to peripheral vasculardisease. In this instance, take the
higher valueas the reference one
|
|
7
|
Measure BP 1 and 5min after assumption ofthe standing position in
elderly subjects, diabeticpatients, and in other conditions in which
posturalhypotension may be frequent or suspected
|
|
8
|
Measure heart rate by pulse palpation (at least30 sec) after the
second measurement in the sittingposition
|
Although some of the aboveadvantages can be obtained by
increasing the number ofoffice BP measurements, 24-hourambulatory BP monitoring
may be useful atthe time of diagnosis and at varying intervals
duringtreatment[40]. Efforts should be made to extend
ambulatory BP monitoring to 24 hours in order to obtaininformation on both
daytimeand night-timeBP profiles, day-night BP difference, morning BP rise and
BP variability.Daytimeand night-time blood pressure values and changes
bytreatment are related to each other, but the prognosticvalue of night-time
blood pressure has been found tobe superior to that of daytime blood
pressure[45,49]. Evidence is also available thatcardiac and
cerebrovascular events have a peak prevalencein the morning,possibly in
relation to thesharp blood pressure rise occurring at awaking fromsleep, as
well as to an increased plateletaggregability, a reduced fibrinolytic activity
and a sympatheticactivation[40,41].
When measuring 24-hour blood pressure[50]
care shouldbe taken to:
· Use only devices validated by international
standardized protocols
· Use cuffs of appropriate size and compare the initial
values with those from a sphygmomanometer to checkthat the differences are not
greater than #177; 5mmHg
· Set the automatic readings at no more than 30 min
intervals to obtain an adequate number of values and have most hours
represented if some readings arerejected because of artefact.
· Automatic deflation of the equipment should be at arate
of no more than 2mmHg/s.
· Instruct the patients to engage in normal activities
but to refrain from strenuous exercise, and to keep the armextended and still
at the time of cuff inflations.
· Ask the patient to provide information in a diary on
unusual events and on duration and quality of nightsleep.
· Obtain another ambulatory BP if the first examination
has less than 70% of the expected number of valid values because of frequent
artefacts. Ensure that the proportion of valid values is similar for the dayand
night periods.
· Remember that ambulatory BP is usually several mmHg
lower than office BP. Different population studies indicate that office values
of 140/90mmHg correspond to average 24-h values of either 125-130mmHg systolic
and 80mmHg diastolic, the corresponding average daytime and night-time values
being 130-135/85 and 120/70mmHg. These values may be regarded as approximate
threshold values for diagnosinghypertension by ambulatory BP. Table II
indicates blood pressure thresholds for the definition of hypertension with
different types of measurement
· Clinical judgement should be mainly based on average
24-hour, day and/or night values. Other information derived from ambulatory
blood pressure (e.g. morning blood pressure surge and blood pressure standard
deviations) is clinically promising, but the field shouldstill be regarded as
in the research phase.
Table II: Blood pressure
thresholds (mmHg) for definition of hypertension with different types of
measurement[40]
|
SBP
|
DBP
|
|
Office or clinic
|
140
|
90
|
|
24-hour
|
125-130
|
80
|
|
Day
|
130-135
|
85
|
|
Night
|
120
|
70
|
|
Home
|
130-135
|
85
|
2. Family and clinical history[40]
A comprehensive family history should be obtained
withparticular attention to hypertension, diabetes, dyslipidaemia,premature
coronary heart disease, stroke, peripheralartery or renal disease.The clinical
history should include: a) duration andprevious levels of high blood pressure;
b) symptomssuggestive of secondary causes of hypertension andintake of drugs or
substances that can raise blood pressure,such as liquorice, nasal drops,
cocaine, amphetamines,oral contraceptives, steroids, nonsteroidal
anti-inflammatory drugs, erythropoietin, and cyclosporin;c) lifestyle factors,
such as dietary intake of fat (animalfat in particular), salt and alcohol,
quantification of smokingand physical activity, weight gain since early
adultlife; d) past history or current symptoms of coronarydisease, heart
failure, cerebrovascular or peripheralvascular disease, renal disease, diabetes
mellitus, gout,dyslipidaemia, asthma or any other significant illnesses,and
drugs used to treat those conditions; e) previousantihypertensive therapy, its
results and adverse effects;and f) personal, family and environmental factors
thatmay influence blood pressure, cardiovascular risk, as wellas the course and
outcome of therapy. Also, physiciansshould enquire after the patient and/or
partner aboutsnoring which may be a sign of sleep apnoea syndromeand increased
cardiovascular risk.
3. Physical examination
In addition to BP, heart rate should be carefullymeasured
(pulse counting over at least 30s or longer ifarrhythmias are reported) because
the repeated findingof values above normal may be an indication of greaterrisk,
increased sympathetic or decreased
parasympatheticactivity[51], or of heart failure. Physical
examinationshould search for evidence of additional risk factors, forsigns
suggesting secondary hypertension, and for evidenceof organdamage. Table III
highlights the physical examination for secondary hypertension, organ damage
and visceral obesity.Waist circumference should be measuredwith the patient
standing and body weight and heightshould be obtained to calculate the body
mass index.
4. Laboratory investigations
Laboratory tests are directed at providing evidencefor
additional risk factors, searching for secondaryhypertension and looking for
the absence or presenceof organ damage. Investigations should progress from
themost simple to the more complicated. The youngerthe patient, the higher the
BP and the fasterthe development of hypertension, the more detailed
thediagnostic work-up should be. However, the minimum laboratory investigations
needed remain a matter ofdebate.
Table III: Physical
examination for secondary hypertension, organ damage and visceral
obesity[40]
|
Signs suggesting secondary hypertension and
organ damage
|
-Features of Cushing syndrome
-Skin stigmata of neurofibromatosis(phaeochromocytoma)
-Palpation of enlarged kidneys (polycystic kidney)
-Auscultation of abdominal murmurs (renovascular
hypertension)
-Auscultation of precordial or chest murmurs (aortic
coarctation or aortic disease)
-Diminished and delayed femoral pulses and
reduced femoral BP (aortic coarctation, aortic
disease)
|
|
Signs of organ damage
|
-Brain: murmurs over neck arteries, motor or
sensory defects
-Retina: fundoscopic abnormalities
-Heart: location and characteristics of apical
impulse, abnormal cardiac rhythms, ventricular
gallop, pulmonary rales, peripheral oedema
-Peripheral arteries: absence, reduction, or asymmetryof pulses,
cold extremities, ischaemic skinlesions
-Carotid arteries: systolic murmurs
|
|
Evidence of visceral obesity
|
-Body weight
-Increased waist circumference (standing position)
M: > 102 cm; F: > 88 cm
-Increased body mass index [body weight (kg)/
height (m)2]
-Overweight =25 kg/m2; Obesity =30
kg/m2
|
Where cardiovasculardiseases are the primary cause of
morbidityand mortality, routine laboratory investigations shouldinclude: blood
chemistry for fasting glucose, total cholesterol,LDL-cholesterol,
HDL-cholesterol, triglycerides(fasting), urate, creatinine, potassium,
haemoglobin andhaematocrit; urinalysis by a dipstick test that permits
thedetection of microalbuminuria; urine microscopic examinationand an
electrocardiogram[40].
Serum creatinine values should be used to estimatecreatinine
clearance via the Cockroft Gault formula[52], easy procedures
allowing identificationof patients with reduced glomerular filtration
andincreased cardiovascular risk but in whom serum creatininevalues are still
in the normal range. When fasting plasma glucose is =5.6 mmol/L(100 mg/dL), a
post-load plasma glucose (glucose tolerancetest) is
recommended[53]. The repeated findingof a fasting plasma
glucose =7.0 mmol/L (126 mg/dL),and an abnormal glucose tolerance test are
consideredindicative of diabetes mellitus[53].
Although highsensitivity C reactive protein (hsCRP)has been
reportedto predict the incidence of cardiovascular events inseveral clinical
settings[54], its added value in determiningtotal
cardiovascular risk is uncertain,except in patients with metabolic syndrome in
whomhsCRP values have been reported to be associatedwith a further marked
increase in risk[55].Table IV gives a summary of the possible
laboratory investigations.
Table IV: Laboratory
investigations[40]
|
Routine tests
|
_ Fasting plasma glucose
_ Serum total cholesterol
_ Serum LDL-cholesterol
_ Serum HDL-cholesterol
_ Fasting serum triglycerides
_ Serum potassium
_ Serum uric acid
_ Serum creatinine
_ Estimated creatinine clearance (Cockroft-Gaultformula) or
glomerular filtration rate (MDRDformula)
_ Haemoglobin and haematocrit
_ Urinalysis (complemented by microalbuminuriavia dipstick test
and microscopic examination)
_ Electrocardiogram
|
|
Recommended tests
|
_ Echocardiogram
_ Carotid ultrasound
_ Quantitative proteinuria (if dipstick test positive)
_ Ankle-brachial BP Index
_ Fundoscopy
_ Glucose tolerance test (if fasting plasma glucose>5.6 mmol/L
(100 mg/dL)
_ Home and 24 h ambulatory BP monitoring
_ Pulse wave velocity measurement (where available)
|
F. MANAGEMENT OF HYPERTENSION
Most of what follows is linked to primary or essential
hypertension in adults.Hypertension may be discovered because of adverse
vascularevents, especially in the eyes, brain, kidneys, orheart, but is more
often asymptomatic and only discoveredon routine measurement of blood
pressure[1,38]. Once diagnosed,decisions have to be made about
the need for treatment.It is well-established that hypertension is a risk
factorfor the development of stroke, heart failure, and renaldamage, and to a
lesser extent ischaemic heart disease, anda reduction in blood pressure is
generally beneficial, althoughmortality remains higher than in
non-hypertensives[56].
Treatment of hypertensionmay involve both non-pharmacological
and pharmacologicalinterventions to reduce blood pressure, as well asassessment
and treatment of any other cardiovascular riskfactors; anyco-existing diseases
should also be treated[3]. Differences inthe detail of
guidelines on the management of hypertensionreflect varying judgements on the
justification for interventionand the relative risks and benefits of
differenttreatments.
1. Non-pharmacological treatment
Adopting a healthylifestyle is beneficial for all individuals,
and any patientwith raised blood pressure should be encouraged to makelifestyle
changes that will reduce their cardiovascular risk.Some of these changes may
also reduce blood pressure,and in those who are at low overall risk no other
treatment may be needed[57,58]. A trial of
non-pharmacologicaltreatment is recommended in most patients beforestarting
drug therapy, but should not unnecessarily delaytreatment, especially if the
patient is at high risk[40,59-61]. Interventionsthat have been
shown to reduce blood pressureinclude[1,3]:
Ø reduction in excess weight
Ø reduction in excess alcohol consumption
Ø reduction in sodium intake
Ø adequate exercise
Ø reduced fat intake
Ø increased fruit and vegetable consumption
Other interventions that have been tried, but with less
evidenceof benefit, include[3]:
Ø increased intake of potassium, magnesium, and
calcium
Ø increased polyunsaturated fat intake with reduced
saturated fat intake
Ø relaxation therapies for stress reduction.
These lifestyle changes may also be promoted in the
populationas a whole, or in individuals most likely to develophypertension, in
strategies for the primary preventionofhigh blood
pressure[1,62].
2. Pharmacological treatment
The main decisions in drugtreatment relate to the blood
pressure at which therapyshould be begun, the target blood pressure, and the
mostappropriate drug regimen to use[3]. Controversies exist in
allthese areas.When to intervenewith antihypertensive drugs dependson factors
including both the measured blood pressure andthe overall cardiovascular risk.
Several guidelines have been published on the measures which entail
pharmacological treatment[40,59,60]:
· Patients with grade 3 hypertension (180/110 mmHg or
higher) should receive prompt drug treatment.
· In grade 2 hypertension, drug therapy is indicated if
blood pressure remains at 160/100 mmHg or higher after a period of lifestyle
modification, which varies depending on the overall level of risk; prompt drug
therapy is advised for those at high or very high risk.
· For patients with grade 1 hypertension, the need for
treatment is less well established; those with associated risk factors should
be given drug therapy if lifestyle modification is inadequate, but some
guidelines suggest that antihypertensives are not indicated in those at lower
risk, or state that priority should be given to those at highest risk.
· Lower thresholds may apply in patients with renal
disease or diabetes, but whether there is any benefit in treating uncomplicated
patients with prehypertension is controversial.
Guidelines therefore generallyrecommend that treatment
decisions should not be basedon age, although slower titration of drugs has
beensuggested[40] in older patients since they may be more
susceptibleto adverse effects. In the very old (those over 80years) the benefit
of starting therapy is less clear[63,64], althougha
study[65] in patients aged 80 years and over found a reduction
in mortality. Those already being treated
shouldcontinue[40,60].
Target blood pressuresare also controversial. The HOT study
found that effective control to maintain the diastolic pressure at about 85
mmHg reduced therate of cardiovascular events, but lower pressures (ofaround 70
mmHg) did not provide any further benefit[66]. Target blood
pressures of below140/90 mmHg[40,61], or below 140/85
mmHg[60] are now recommended;lower targets may be considered
if toleratedby the patient, particularly in patients at high
risk[40]. A lowertarget of below 130/80 mmHg has also been
suggested for patients with established ischaemic heart
disease[67], andlower targets may also be appropriate in
diabetics and patients with renal disease.
Antihypertensive drugs comprise several classes of active
pharmaceutical ingredients (APIs) with the therapeutic objective of controlling
hypertension. Table V shows the different classes and subclasses of
antihypertensives.
Table V: Classes and
subclasses of antihypertensive medications with common examples[68]
|
CLASS
|
EXAMPLES
|
|
Targeting renin-angiotensin system
|
|
Angiotensin-converting
enzyme inhibitors
|
Captopril, lisinopril, ramipril
|
|
Angiotensin receptor
antagonists
|
Candesartan, losartan, valsartan
|
|
Direct renin antagonists
|
Aliskiren
|
|
Adrenoceptor antagonists
|
|
â-Blockers
|
Atenolol, metoprolol, propranolol
|
|
á-Blockers
|
Doxazosin, labetalol (also a â-blocker),
phentolamine, phenoxybenzamine
|
|
Calcium channel blockers
|
|
Phenylalkylamine
|
Verapamil
|
|
Dihydropyridines
|
Amlodipine, nifedipine, nimodipine
|
|
Benzothiazepines
|
Diltiazem
|
|
Diuretics
|
|
Thiazides
|
Bendroflumethiazide,
hydrochlorothiazide
|
|
Loop
|
Furosemide, bumetanide
|
|
Potassium sparing/
aldosterone antagonist
|
Amiloride, spironolactone
|
|
Vasodilators
|
Hydralazine, minoxidil
|
|
Centrally acting agents
|
Clonidine, methyldopa
|
|
Ganglion block
|
Trimetaphan
|
The classes of antihypertensive drugs differ in their chemical
structures thence their varying functions. Antihypertensive drugs are
frequently used in other unrelated conditions, for
example, â-blockers
in thyrotoxicosis[69]and anxiety[70], or
angiotensin-converting enzyme inhibitors (ACEIs) in heart failure.
The following subsections will focus on the applied
pharmacology of agents used in the management of hypertension, some of their
side-effects, as well as some drug interactions.
o Drugs which target the renin-angiotensin system
(RAS)
Three drug classes directly target points of the RAS pathway.
They act to reduce production of the peptide hormone angiotensin II, or reduce
its receptor binding. Figure 6 shows the different sites of action of drugs
affecting the renin-angiotensin system.
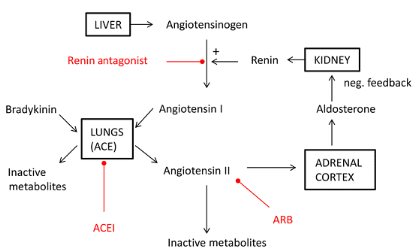
Figure 6: Sites of action
of drugs affecting the renin-angiotensin system.[68]
Angiotensin II has high affinity for AT1 G-protein-coupled
receptors, activation of which causes increased arteriolar tone and systemic
vascular resistance (SVR). It also causes sympathetic nervous system
activation, increased pituitary secretion of antidiuretic and
adrenocortocotrophic hormones, and increased adrenocortical secretion of
aldosterone[71].By antagonizing the RAS pathway, SVR and
arterial pressure are reduced. This effect is potentiated by a reduction in
aldosterone secretion with resultant reduction in renal sodium and water
retention. Negative feedback results in increased renin release by the
juxtaglomerular apparatus.
1. ACEI drugs[3,68,71-73]
The discovery that the venom of the Brazilian pit viper, which
causes a massive decrease in arterial pressure, works by inhibition of
angiotensin-converting enzyme (ACE) led to the development of synthetic, orally
administered ACEIs. ACEIs are among the first-line treatment in non-black
patients under 55 years of age with primary hypertension.They are also
indicated in heart failure, post-myocardial infarction, diabetic nephropathy,
and chronic kidney disease (although not acute kidney injury). The renaland
cardiac protective effects of ACEIs are greater than those expected by arterial
pressure control alone.
ACE is a metallopeptidase enzyme which occurs mainly within
the pulmonary vasculature. The inhibition of ACE reduces the cleavage of the
decapeptide hormone angiotensin I to the octapeptide angiotensin IIand reduces
metabolism of the peptide bradykinin to inactivesubstances. The reduction in
angiotensin II is responsible formost of the therapeutic effects.
v Perindopril
o Chemical structure
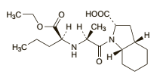 C19H32N2O5 C19H32N2O5
o Pharmaceutical form and administration
Perindopril is available as oral tablets and when taken as the
erbumine salt should be taken before food. Perindopril is also available as the
arginine salt; 5 mg ofperindopril arginine is equivalent to about 4 mg
ofperindopril erbumine.In the treatment of hypertension perindopril is givenin
an initial dose of 4 mg of the erbumine or 5 mg of thearginine salt once
daily.
o Pharmacokinetic data
Perindopril acts as a prodrug of the diacid perindoprilat, its
active form. After oral doses perindopril is rapidly absorbed with a
bioavailability of about 65 to 75%. It is extensively metabolised, mainly in
the liver,to perindoprilat and inactive metabolites including glucuronides. The
presence of food is reported to reducethe conversion of perindopril to
perindoprilat. Peakplasma concentrations of perindoprilat are achieved 3to 4
hours after an oral dose of perindopril. Perindoprilat is about 10 to 20% bound
to plasma proteins. Perindopril is excreted predominantly in the urine,
asunchanged drug, as perindoprilat, and as other metabolites. The elimination
ofperindoprilat is biphasic witha distribution half-life of about 5 hours and
an elimination half-life of 25 to 30 hours or longer, the latter half-life
probably representing strong binding to angiotensin-converting enzyme. The
excretion of perindoprilat is decreased in renal impairment.
o Pharmacodynamic data
Perindopril, as well as other ACE inhibitors, inhibit ACE,
which isinvolved in the conversion of angiotensin I to angiotensin II.
Angiotensin II stimulates the synthesis andsecretion of aldosterone and raises
blood pressure via apotent direct vasoconstrictor effect.The pharmacological
actions of ACEinhibitors are thought to be primarily due to the inhibition of
the renin-angiotensin-aldosterone system, butsince they also effectively reduce
blood pressure in patients with low renin concentrations other mechanismsare
probably also involved.
o Clinical pharmacology
The accumulation of bradykininhas some therapeutic advantage
through vasodilatation, but isalso responsible for a dry cough in susceptible
individuals.
ACEIs can also precipitate renal dysfunction by decreasing
renal efferent arteriolar tone, thereby decreasing effective renal perfusion
pressure, a particular risk in renal artery stenosis. Otherside-effects include
hyperkalaemia due to reduced aldosterone secretion, agranulocytosis, skin
rashes, and taste disturbance. A rare idiosyncratic reaction to ACEIs can cause
angioedema with potential upper airway obstruction; this can occur several
years after initiation of ACEI therapy. ACEIs are contraindicatedin pregnancy
as they are associated with birth defects. ACEIs may interactwith drugs used
perioperatively. For example, non-steroidal anti-inflammatory drugs can
precipitaterenal dysfunction in combination with ACEIs. They can also reduce
the efficacy of ACEIs by decreasing prostaglandin synthesis.Interactions with
diuretics may cause hypovolaemia and hyponatraemia, while concurrent use of
potassium supplements orpotassium-sparing diuretics may result in
hyperkalaemia.Drugs which are renally excreted (e.g. digoxin and lithium) may
accumulatein patients taking ACEIs.
2. ARA drugs[3,71,74]
ARAs are commonly used in patients who are intolerant to
ACEIsas they are less likely to cause a dry cough.
v Losartan
o Chemical structure
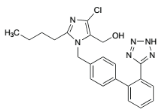 C22H22ClKN6O C22H22ClKN6O
o Pharmaceutical form and administration
Losartan is given orally as the potassium salt in tablet and
sachet forms.In hypertension the usual dose of losartan potassiumis 50 mg once
daily. The dose may be increased, if necessary, to 100 mg daily as a single
dose or in two divided doses. An initial dose of 25 mg once daily should
begiven to patients with intravascular fluid depletion, and is recommended in
the UK in patients over 75 years ofage. Similar reductions may be appropriate
in patients with hepatic or renal impairment
o Pharmacokinetic data
Losartan is readily absorbed from the gastrointestinal tract
after oral doses, but undergoes substantial firstpass metabolism resulting in a
systemic bioavailability of about 33%. It is metabolized to an active
carboxylic acid metabolite E-3174 (EXP-3174), which has greater pharmacological
activity than losartan; some inactive metabolites are also formed. Metabolism
is primarilyby cytochrome P450 isoenzymes CYP2C9 and CYP3A4. Peak plasma
concentrations of losartan andE-3174 occur about 1 hour and 3 to 4 hours,
respectively, after an oral dose. Both losartan and E-3174 aremore than 98%
bound to plasma proteins. Losartan isexcreted in the urine, and in the faeces
via bile, asunchanged drug and metabolites. About 4% of an oraldose is excreted
unchanged in urine and about 6% is excreted in urine as the active metabolite.
The terminal elimination half-lives of losartan and E-3174 are about1.5 to 2.5
hours and 3 to 9 hours, respectively.
o Pharmacodynamic data
Losartan is a competitive angiotensin II receptor antagonist
with antihypertensive activity due mainly to selectiveblockade of AT1 receptors
and the consequent reducedpressor effect of angiotensin II.
o Clinical pharmacology
The therapeutic andside-effects are broadly similar to those
of ACEIs, with evidenceof reduced risk of new onset diabetes, stroke,
progression of cardiac failure, and all-cause mortality in patients with
chronic kidney disease.Direct targeting of angiotensin II receptors has
theoretical advantages over ACE inhibition. Angiotensin II may be
producedthrough non-ACE pathways, for example, by the enzyme chymase in kidney
tissue, which is not affected by ACEIs. ARAs do not inhibit bradykinin
metabolism, and therefore, the incidence of cough is much less than with ACEIs.
The risk of angiooedema is greatly reduced with ARAs compared with ACEIs.
Losartan is contra-indicated in pregnancy.It should be used with caution in
patients with renal artery stenosis. Losartan is excreted in urine and in
bileand reduced doses may therefore be required in patients with renal
impairment and should be consideredin patients with hepatic impairment.
Patients with volume depletion (for example those who have receivedhigh-dose
diuretic therapy) may experience hypotension; volume depletion should be
corrected beforestarting therapy, or a low initial dose should be used.Since
hyperkalaemia may occur, serum-potassium concentrations should be monitored,
especially in theelderly and patients with renal impairment, and
potassium-sparing diuretics should generally be avoided.
3. Direct renin inhibitors (DRIs)[3,68]
v Aliskiren
Aliskiren, a piperidine derivative, is the only available drug
in this
class and is used by specialists in patients who are unresponsive
to, or intolerant of, other antihypertensives.
o Chemical structure
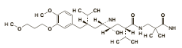 (C30H53N3O6)2,C4H4O4 (C30H53N3O6)2,C4H4O4
o Pharmaceutical form and administration
Aliskiren is given as the fumarate. Doses are expressed in
terms of the base; 165.8 mg of aliskiren fumarate is equivalent to about150 mg
of aliskiren. The usual initial oral dose of aliskiren is 150 mg once daily,
increased to 300 mg oncedaily if necessary. Doses may be taken before or
afterfood, but patients should establish a routine patternwith regard to
meals.
o Pharmacokinetic data
Aliskiren is poorly absorbed from the gastrointestinal tract
with a bioavailability of about 2.5%. Peak plasma concentrations are reached
about 1 to 3 hours after anoral dose. Absorption is reduced when aliskiren is
taken with a high-fat meal. Aliskiren is about 50% boundto plasma proteins. It
is excreted mainly in the faeces,possibly via the bile; about 25% of the
absorbed doseis excreted in the urine as unchanged drug. Aliskiren is a
substrate for the cytochrome P450 isoenzymeCYP3A4 but metabolism appears to be
minimal. The elimination half-life is about 24 to 40 hours, and steady-state
concentrations are reached in about 7 to 8days.
o Pharmacodynamic data
Aliskiren directly inhibits the enzyme renin, which is
secreted by granular cells of the juxtaglomerular apparatus. Renin inhibition
reduces theconversion of the hepatically secreted polypeptide angiotensinogen
to angiotensin I.Its effect on the RAS is therefore `upstream' of ACEIs and
ARAs and it does not cause bradykinin accumulation.
o Clinical pharmacology
DRIs have the same potential to cause renal dysfunction and
electrolyte disturbances as ACEIs and ARAs. It should therefore be used with
caution in patients with renal impairment or renovascular hypertension.
Patients withsodium or volume depletion (for example those receiving high-dose
diuretics) may experience symptomatic hypotension on starting aliskiren and
treatment shouldbegin under close medical supervision.Diarrhea is aspecific
side-effect to higher doses of DRIs. Aliskiren may have a larger role in the
management ofhypertension in future, possibly in combination with other drugs.
Aliskiren should be avoided in pregnancy since drugsacting on the
renin-angiotensin system have been associated with fetal and neonatal morbidity
and mortality.
Use of aliskiren with other antihypertensives or drugsthat
cause hypotension may have an additive effect.Renal function and electrolytes
should be monitored indiabetic patients taking aliskiren and ACE
inhibitorssince there is an increased risk of hyperkalaemia andrenal
impairment.Aliskiren is metabolised to a small extent by the cytochrome P450
isoenzyme CYP3A4 but few significant interactions have been reported.
Plasma-aliskiren concentrations may be reduced by irbesartan and increasedby
atorvastatin and ketoconazole but the clinical relevance is not clear.
Aliskiren has caused significant decreases in furosemide concentrations.
4. Adrenoceptor antagonists
a) â-Blockers[3,68,71,74]
â-Blockers are not used as first-line antihypertensives
unless there are otherindications, for example, after myocardial infarction, or
in tachyarrhythmias such as atrial fibrillation. Theirdiverse indications
include stable heart failure, thyrotoxicosis, oesophageal varices, anxiety, and
glaucoma.
â-Blockers antagonize catecholamines at
â-adrenoceptors.
These Gs type G-protein-coupled receptors are
classified as â1, present mainly within the heart and kidneys; and
â2, present throughout the body in lungs, blood vessels, and muscle. The
reduction in arterial pressure achieved by â-blockers is
attributable
to their effects upon multiple pathways. Block of â1
receptors in
the sinoatrial node reduces heart rate and block of myocardial
receptors reduces contractility (reduced chronotropy and inotropy,
respectively). They also reduce sympathetic nervous system activity, while
block of receptors in the juxtaglomerular apparatus reduces renin secretion.
v Propranolol
o Chemical structure
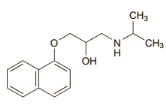 C16H21NO2,HCl C16H21NO2,HCl
o Pharmaceutical form and administration
Propranolol hydrochloride is usually given orally.
Inhypertension it is given in initial doses of 40 to 80 mgtwice daily increased
as required to a usual range of 160 to 320 mg daily; some patients may require
up to640 mg daily.
o Pharmacokinetic data
Propranolol is almost completely absorbed from
thegastrointestinal tract, but is subject to considerablehepatic-tissue binding
and first-pass metabolism. Peakplasma concentrations occur about 1 to 2 hours
after anoral dose. Plasma concentrations vary greatly between individuals.
Propranolol has high lipid solubility. Itcrosses the blood-brain barrier and
the placenta, and is distributed into breast milk. Propranolol is about 90%
bound to plasma proteins. It is metabolised in the liverand at least one of its
metabolites (4-hydroxypropranolol) is considered to be active, but the
contribution of metabolites to its overall activity is uncertain.The
metabolites and small amounts of unchanged drug are excreted in the urine. The
plasma half-life of propranolol is about 3 to 6 hours.
o Pharmacodynamic data
Propranolol is a non-cardioselective â-blocker.
Propranolol also blocks sodium channels andhave membrane stabilizing activity
and is thus classed as Vaughan-Williams class 2 antiarrhythmic with other
â-blockers. In addition to their antihypertensive effect, propranolol
improves the myocardial oxygen supply:demand ratio and help reduce myocardial
ischemiaby prolonging the period of diastole.
o Clinical pharmacology
While â-blockers are used instable heart failure, they
have the potential to worsen symptomsin some patients by reducing cardiac
output. Poor peripheralcirculation and Raynaud's phenomenon may be
precipitatedboth by reduced cardiac output and block of peripheral â2
receptors. Bronchospasm caused by â2 block may be a
significantrespiratory side-effect in susceptible individuals, for
example,asthmatics. Central nervous system effects include malaise,tiredness,
and vivid dreams, particularly with lipid-solubledrugs. Ininsulin-dependent
diabetic patients, the symptoms ofhypoglycaemia may be suppressed by
sympathetic block.
b) á-Blockers[3,68,71]
á-Blockers are used to treat hypertension in patients
resistantto, or intolerant of, other treatments. Specific indications fortheir
use in secondary hypertension include labetalol for preeclampsia and
phentolamine in the perioperative management of phaeochromocytoma.
á-blockers are also commonly used to improve urinary flow in benign
prostatic hyperplasia, for
example, tamsulosin.
v Prazosin
o Chemical structure
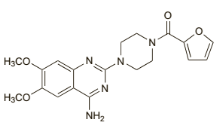 C19H21N 5O 4,HCl C19H21N 5O 4,HCl
o Pharmaceutical form and administration
Prazosin is given orally as the hydrochloride, but dosesare
usually expressed in terms of the base. Prazosin hydrochloride 1.1 mg is
equivalent to about 1 mg of prazosin.In hypertension, the usual initial dose
is500 micrograms two or three times daily for 3 to 7days; if tolerated the dose
may then be increased to1 mg two or three times daily for a further 3 to 7
days,and thereafter gradually increased, according to the patient's response,
to a usual maximum of 20 mg daily individed doses.
o Pharmacokinetic data
Prazosin is readily absorbed from the gastrointestinaltract
with peak plasma concentrations occurring 1 to 3hours after an oral dose. The
bioavailability is variableand a range of 43 to 85% has been reported.
Prazosinis highly bound to plasma proteins. It is extensivelymetabolised in the
liver and some of the metabolites are reported to have hypotensive activity. It
is excretedas the metabolites and 5 to 11% as unchanged prazosinmainly in the
faeces via the bile. Less than 10% is excreted in the urine. Small amounts are
distributed intobreast milk. Its duration of action is longer than wouldbe
predicted from its relatively short plasma half-life ofabout 2 to 4 hours.
Half-life is reported to be increasedto about 7 hours in patients with heart
failure.
o Pharmacodynamic data
Prazosin is an alpha blocker that acts by selective blockade
of alpha1-adrenoceptors.Prazosin produces peripheral dilatation of both
arterioles and veins and reduction of peripheral resistance,usually without
reflex tachycardia. It reduces bothstanding and supine blood pressure with a
greater effect on the diastolic pressure.
o Clinical pharmacology
Treatment with prazosin should be introduced cautiously
because of the risk of sudden collapse following the initial dose. Extra
caution is necessary in patients with hepatic or renal impairment and in
theelderly.Prazosin is not recommended for the treatment of heart failure
caused by mechanical obstruction, for exampleaortic or mitral valve stenosis,
pulmonary embolism,and restrictive pericardial disease. It should be used with
caution in patients with angina pectoris. Prazosinmay cause drowsiness or
dizziness; patients so affected should not drive or operate machinery.The
hypotensive effects of prazosin may be enhancedby use with diuretics and other
antihypertensives, andby alcohol and other drugs that cause hypotension.
Therisk of first-dose hypotension may be particularly increased in patients
receiving beta blockers or calcium-channel blockers.
5. Calcium channel blockers
(CCBs)[3,68,71,74]
CCBs are first-line treatment for primary hypertension in
patients over the age of 55 and black patients of African orCaribbean family
origin. Rate-controlling CCBs (diltiazem, verapamil) are also used to manage
tachyarrhythmias and angina,where their negative inotropic and chronotropic
effects improvethe myocardial oxygen supply. Some CCBs havespecific non-cardiac
indications, for example, nimodipine inneurosurgery to reduce cerebralvasospasm
in patients afterspontaneous subarachnoid hemorrhage, and verapamil inneurology
to treat cluster headache.
v Amlodipine
o Chemical structure
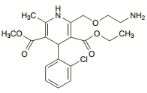 C20H25ClN2O5,C6H6O3S C20H25ClN2O5,C6H6O3S
o Pharmaceutical form and administration
Amlodipine is given orally as the besilate, but doses are
usually expressed in terms of the base; amlodipine besilate 6.9 mg is
equivalent to about 5 mg of amlodipine. The camsilate, maleate, and mesilate
are alsoused.In hypertension the usual initial dose is 5 mg once daily,
increased, if necessary, to 10 mg once daily.
o Pharmacokinetic data
Amlodipine is well absorbed after oral doses with peakblood
concentrations occurring after 6 to 12 hours. Thebioavailability varies but is
usually about 60 to 65%.Amlodipine is reported to be about 97.5% bound toplasma
proteins. It has a prolonged terminal elimination half-life of 35 to 50 hours
and steady-state plasmaconcentrations are not achieved until after 7 to 8
daysof use. Amlodipine is extensively metabolized in theliver; metabolites are
mostly excreted in urine togetherwith less than 10% of a dose as unchanged
drug.
o Pharmacodynamic data
Amlodipine as well as other dihydropyridines act on L-type
calcium channels present in vascularsmooth muscle and in myocardial and nodal
tissues. The variable affinity of the different CCBs to these different tissues
determines their effects.
o Clinical pharmacology
Cardiovascular side-effects include reflex tachycardia which
may potentiate myocardial ischemia, disturbance of the peripheral
microcirculation leading to swelling of the hands and feet, flushing, and
headache. Rate-limiting agents prolongatrioventricular conduction and cause
bradycardia; the negativeinotropic and chronotropic effects may worsen heart
failure. Amlodipine may enhance the antihypertensive effects ofother
antihypertensive drugs such as beta blockers although the combination is
generally well tolerated. Enhanced antihypertensive effects may also be seen
ifused with drugs such as aldesleukin and antipsychotics that cause
hypotension. Amlodipine may modify insulinand glucose responses and therefore
diabetic patientsmay need to adjust their antidiabetic treatment when receiving
amlodipine. Amlodipine is extensively metabolized in the liver by the
cytochrome P450 isoenzymeCYP3A4, and interactions may occur with other
drugs,such as quinidine, sharing the same metabolic pathway, and with enzyme
inducers, such as carbamazepine, phenytoin, and rifampicin, and
enzymeinhibitors, such as cimetidine, erythromycin, and HIVprotease
inhibitors.
6. Diuretics[3,68,71,72,74]
Thiazide (bendroflumethiazide, hydrochlorothiazide) and
thiazide-like (chlortalidone, indapamide) diuretics are the most commonly
prescribed diuretic agents used to treat hypertension.They are used in patients
intolerant of CCBs and in patients with heart failure, or at risk of heart
failure. They are also usedas `add on' drugs in patients who have not responded
to firstand second-line antihypertensive treatments.
o Chemical structure
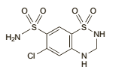 C7H8ClN3O4S2 C7H8ClN3O4S2
o Pharmaceutical form and administration
Thiazides are usuallygiven in the morning so that sleep is not
interrupted by diuresis.Hydrochlorothiazide is given orally.In the treatment of
hypertension an initial dose of12.5 mg may be sufficient, increasing to 25 to
50 mgdaily if necessary, either alone or with other antihypertensives. Doses of
up to 100 mg have been suggestedbut are rarely necessary.
o Pharmacokinetic data
Hydrochlorothiazide is fairly rapidly absorbed fromthe
gastrointestinal tract. It is reported to have a bioavailability of about 65 to
70%. It has been estimated tohave a plasma half-life of between about 5 and
15hours and appears to be preferentially bound to redblood cells. It is
excreted mainly unchanged in theurine. Hydrochlorothiazide crosses the
placental barrier and is distributed into breast milk.
o Pharmacodynamic data
Thiazides are moderately potent diuretics and exerttheir
diuretic effect by reducing the reabsorption ofelectrolytes from the renal
tubules, thereby increasing the excretion of sodium and chloride ions, and
consequently of water. They act mainly at the beginning ofthe distal tubules.
The excretion of other electrolytes,notably potassium and magnesium, is also
increased.The excretion of calcium is reduced. They also reduce
carbonic-anhydrase activity so that bicarbonate excretion is increased, but
this effect is generally small compared with the effect on chloride excretion
and does notappreciably alter the pH of the urine. They may also reduce the
glomerular filtration rate.Their hypotensive effect is probably partly due to a
reduction in peripheral resistance; they also enhance theeffects of other
antihypertensives. Paradoxically, thiazides have an antidiuretic effect in
patients with diabetes insipidus.
o Clinical pharmacology
Thiazide diuretics have many clinically relevant
biochemicalside-effects including hypokalaemia, hypercalcaemia, hyponatraemia,
hypomagnesaemia, hyperglycaemia, hyperuricaemia, hypercholesterolaemia, and
hypochloraemic alkalosis. Plasma volume loss may precipitate dehydration and
acute kidney injury. Less common side-effects include skin rashes,
photosensitivity reactions, and blood dyscrasias including
thrombocytopaenia.
Many of the interactions of hydrochlorothiazide andother
thiazides are due to their effects on fluid and electrolyte balance.
Diuretic-induced hypokalaemia mayenhance the toxicity of digitalis glycosides
and mayalso increase the risk of arrhythmias with drugs that prolong the QT
interval, such as astemizole, terfenadine, halofantrine, pimozide, and sotalol.
Thiazidesmay enhance the neuromuscular blocking action of competitive
neuromuscular blockers, such as atracurium, probably by their hypokalaemic
effect. The potassium-depleting effect of diuretics may be enhanced
bycorticosteroids, corticotropin, beta2 agonists such as salbutamol,
carbenoxolone, amphotericin B, or reboxetine.
Diuretics may enhance the effect of other antihypertensives,
particularly the first-dose hypotension that occurs with alpha blockers or ACE
inhibitors. Orthostatichypotension associated with diuretics may be enhanced by
alcohol, barbiturates, or opioids. The antihypertensive effects of diuretics
may be antagonised bydrugs that cause fluid retention, such as
corticosteroids,NSAIDs, or carbenoxolone; diuretics may enhance the
nephrotoxicity of NSAIDs. Thiazides have been reported to diminish the response
to pressor amines, suchas noradrenaline, but the clinical significance of this
effect is uncertain.Thiazides should not usually be used with lithium sincethe
association may lead to toxic blood concentrations of lithium. Other drugs for
which increased toxicity hasbeen reported when given with thiazides include
allopurinol and tetracyclines. Thiazides may alter the requirements for
hypoglycaemics in diabetic patients.
Other diuretics include aldosterone antagonists, for example,
spironolactone, are recommended as fourth-line treatment of primary
hypertension. The use of these drugs carries a risk of hyperkalaemia,
particularly in patients with impaired renal function or who are taking other
potassium-sparing agents. Loop diuretics are indicated for resistant
hypertension in patients with heart failure, chronic kidney disease, and in
those at risk of hyperkalaemia.
· Other antihypertensives
1. Vasodilators[3,68,71]
Directly acting vasodilators, for example, hydralazine
andminoxidil, are seldom used due to their side-effect profiles.Hydralazine is
used in hypertension secondary to pre-eclampsia. In addition to its
antihypertensive effects, minoxidil is used topically as a treatment for male
pattern baldness.
v Minoxidil
o Chemical structure
 C9H15N5O C9H15N5O
o Pharmaceutical form and administration
In the treatment of hypertension minoxidil is givenwith a beta
blocker, or with methyldopa, to diminishthe cardiac-accelerating effects, and
with a diuretic,usually a loop diuretic, to control oedema.An initial dose of 5
mg of minoxidil daily(or 2.5 mg daily in the elderly) is gradually increased
atintervals of not less than 3 days to 40 or 50 mg dailyaccording to response;
in exceptional circumstances up to 100 mg daily has been given.
In the treatment ofalopecia androgenetica (male-pattern
baldness) 1 ml of a 2% or 5% solution of minoxidil is applied twice daily to
the scalp. The 5% solutionis not recommended for women.
o Pharmacokinetic data
About 90% of an oral dose of minoxidil is absorbedfrom the
gastrointestinal tract. The plasma half-life isabout 4.2 hours although the
haemodynamic effectmay persist for up to 75 hours, presumably due to
accumulation at its site ofaction. Minoxidil is not boundto plasma proteins. It
is distributed into breast milk.Minoxidil is extensively metabolised by the
liver. It requires sulfation to become active, but the major metabolite is a
glucuronide conjugate. Minoxidil is excretedpredominantly in the urine mainly
in the form ofmetabolites. Minoxidil and its metabolites are dialysable,
although the pharmacological effect is not reversed. About 0.3 to 4.5% of a
topical dose of minoxidil is absorbed from intact scalp.
o Pharmacodynamic data
Vasodilators cause relaxation of vascular smooth muscle in
resistance (arteriolar) vessels. Minoxidil achieves this via adenosine
triphosphate-dependent potassium channels on smoothmuscle cell
membranes.Vasodilatation provokes reflex cardiac stimulation (which may
precipitate cardiac ischemia) and RAS activation. These compensatory responses
may be offset by â-blockersor diuretics.
o Clinical pharmacology
Vasodilator drugs are poorly tolerated. Side-effects
includeheadache, fluid retention, and edema. Other specific side effects
include left ventricular hypertrophy, pericardial and
pleural effusions,
hypertrichosis and coarsening of featureswith minoxidil, while peripheral
neuropathy, blood dyscrasias,and a lupus-like reaction can occur with
hydralazine.The antihypertensive effect of minoxidil may be enhanced by use of
other hypotensive drugs. Severeorthostatic hypotension may occur if minoxidil
andsympathetic blocking drugs such as guanethidine aregiven
concurrently.Topical minoxidil should not be used with other topicalagents
known to enhance absorption, such as corticosteroids, retinoids, or occlusive
ointment bases.
2. Centrally acting agents[3,68,71,74]
Centrally acting agents include clonidine (á2
adrenoceptor agonist), methyldopa (precursor of an á2 adrenoceptor
agonist), and moxonidine (agonist at imidazoline binding sites). Their use
inprimary hypertension is limited to difficult to treat cases, while methyldopa
is used to treat hypertension in pregnancy. The evidence base for the use of
centrally acting drugs in hypertension is limited and adverse effects are
common. Clonidine is an analgesic and sedative drug which reduces the
minimumalveolarconcentration of inhalation anestheticagents. Both of these
drugs cause side-effects including drymouth and sedation. Methyldopa has
immunological side effects, including pyrexia, hemolytic anemia, and
hepatitis.Cessation of treatment with clonidine can cause
reboundhypertension.
v Methyldopa
o Chemical structure
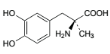 C10H13NO4,1 / H2O C10H13NO4,1 / H2O
o Pharmaceutical form and administration
Methyldopa is given orally as the sesquihydrate, butdoses are
usually expressed in terms of anhydrousmethyldopa. Methyldopa sesquihydrate
1.13 g isequivalent to about 1 g of anhydrous methyldopa. Forhypertensive
crises, methyldopa has been given intravenously as methyldopate
hydrochloride.In hypertension, the usual initial adult oral dose is250 mg of
methyldopa two or three times daily for 2days; this is then adjusted, not more
frequently than every 2 days according to response, up to a usual maximum dose
of 3 g daily. The usual maintenance dosage is 0.5 to 2 g of methyldopa daily.
In the elderly an initial dose of 125 mg twice daily has been used; this
dosemay be increased gradually if necessary, but should not exceed 2 g daily
o Pharmacokinetic data
After oral use methyldopa is variably and
incompletelyabsorbed, apparently by an amino-acid active transportsystem. The
mean bioavailability has been reported to be about 50%. It is extensively
metabolised and is excreted in urine mainly as unchanged drug and the Osulfate
conjugate. It crosses the blood-brain barrier andis decarboxylated in the CNS
to active alpha-methylnoradrenaline.The elimination is biphasic with a
half-life of about 1.7 hours in the initial phase; the second phase is more
prolonged. Clearance is decreased and half-life prolongedin renal impairment.
Plasma protein binding is reported to be minimal. Methyldopa crosses the
placenta; smallamounts are distributed into breast milk.
o Pharmacodynamic data
Methyldopa is an antihypertensive that is thought tohave a
mainly central action. It is decarboxylated in theCNS to
alpha-methylnoradrenaline, which is thoughtto stimulate alpha2 adrenoceptors
resulting in a reduction in sympathetic tone and a fall in blood pressure.
Itmay also act as a false neurotransmitter, and have some inhibitory actions on
plasma renin activity. Methyldopa reduces the tissue concentrations of
dopamine,noradrenaline, adrenaline, and serotonin.
o Clinical pharmacology
Methyldopa should be used with caution in the elderly,and in
patients with hepatic or renal impairment or witha history of haemolytic
anaemia, liver disease, or depression. Care is also advisable in patients with
Parkinsonism. It should not be given to patients with active liver disease or
depression and it is not recommendedfor phaeochromocytoma.It is advisable to
make periodic blood counts and toperform liver function tests at intervals
during the first6 to 12 weeks of treatment or if the patient develops
anunexplained fever. Patients taking methyldopa mayproduce a positive response
to a direct Coombs' test; if blood transfusion is required, prior knowledge of
apositive direct Coombs' test reaction will aid crossmatching. Methyldopa may
cause sedation; if affected, patients should not drive or operate machinery.
The hypotensive effects ofmethyldopa are potentiatedby diuretics, other
antihypertensives, and drugs withhypotensive effects. However, there have been
reportsof paradoxical antagonism of the hypotensive effectsby tricyclic
antidepressants, antipsychotics, and betablockers. Sympathomimetics may also
antagonise the hypotensive effects.There may be an interaction between
methyldopa andMAOIs and care is required if they are given together.Caution is
also needed with catechol-O-methyltransferase inhibitors, such as entacapone,
since they might reduce the metabolism of methyldopa.
3. Ganglion blockers[3,68]
Ganglion blockers, such as trimetaphan, antagonize
acetylcholine at nicotinic receptors, including those at the adrenal cortex.
Trimetaphan causes vasodilatation with a consequent rapid reduction in arterial
pressure. Although ganglion blockers may be
used to manage hypertensive
crises or to provide hypotensive anesthesia, their use is increasingly rare.
The drug regimenmay include drugs with differing
pharmacological actions; the antihypertensive mechanism is not fully understood
in all cases. Historically, thiazide diuretics and beta blockers have been the
mainstay of drug therapy for hypertension, but CCBs, ACEI, ARAs, and alpha
blockers are now also widely used[3].
Studies such as the TOMHS[75] (comparing
chlortalidone, acebutolol, amlodipine, enalapril, and doxazosin), and a similar
study[76] (comparing hydrochlorothiazide, atenolol, diltiazem,
captopril, prazosin, and clonidine), have shown that the main types of
antihypertensive drug reduce blood pressure to a similar extent and in a
similar proportion of patients, although the response may also depend on
individual factors such as age[77] and
race[78,79]. ARAs also effectively reduceblood pressure.
However, it is now generally acknowledgedthat a single drug is unlikely to
control blood pressureadequately and most patients will require more thanone
drug to reach their treatment target. Tolerance of thedrug groups is also
similar, although there has been concernabout the metabolic effects of
thiazides and betablockers. Alpha blockers (specifically
doxazosin[80]) havebeen associated with an increased risk of
heart failure,which may limit their use. The safety of short-acting
dihydropyridine CCBs has also been questioned,and they are no longer generally
recommended forhypertension[3]; long-acting
dihydropyridines,however, are of established benefit[81].
Diuretics(particularly thiazides) and beta blockers were the firstdrugs to
demonstrate an effect on mortality in long-termoutcome studies and have
therefore been preferred for initialtherapy[3]. However,
long-term studies with other druggroups have now been performed, and have
generallyshown comparable effects on mortality and morbidity. Ameta-analysis
concluded that there was little differencein overall cardiovascular outcomes
for regimens based on ACEIs, ARAs, CCBs, beta blockers, or diuretics,
suggestingthe major benefit of treatment related to reduction of blood pressure
rather than to specific properties of the individualdrugs[82].
In general, guidelines acknowledge that lowering bloodpressure appears to be
more important than which drug ischosen for initial therapy, and that most
patients will requirea combination of drugs, making the initial choice
lessimportant[3]. Thiazide diuretics, ACEIs, ARAs, or CCBs
mayall be used, and choice should take into account individualpatient
characteristics, including age, ethnicity, contra-indicationsor compelling
indications for specific drugs, adverseeffects, and relative
cost-effectiveness[40,59-61]. Strictguidance is therefore not
generally given, although foruncomplicated patients WHO
guidelines[59]recommend thiazide diureticsas first-line,
whereas in theUK[81] diuretics or CCBsare recommendedfor older
patients (55 years or over) and black patients,while in younger, non-black
patients ACEIs or ARAsare preferred. Compellingindications in all the
guidelines include the use of ACEIs or ARAs in patientswith nephropathy,
diuretics or CCBs in elderly patients, and beta blockers in patientswho have
had a myocardial infarction.
Having decided what drug to use, treatment is started at
thelowest recommended dose. If this is ineffective or onlypartially effective
the dose may be increased (except in thecase of thiazide diuretics where there
is generally no additionalbenefit, but more adverse effects);
alternativelyanother first-line drug may either be substituted (sequential
therapy) or added (combination therapy). Two-drugcombinations will control
blood pressure in a higher proportionof patients and may be necessary in most
patientsto achieve optimal levels, although the effects of the twodrugs may not
be fully additive. Combination therapy alsoallows lower doses of the individual
drugs to be used witha consequent reduction in adverse effects. Initial
treatmentwith a low-dose combination may be considered in
somepatients[40,61].
The most effective combinations involve drugsthat act on
different physiological systems. Appropriatecombinations therefore
include[3]:
Ø diuretic plus beta blocker
Ø diuretic plus ACEI
Ø diuretic plus ARA
Ø CCB plus ACEI
Ø CCB plus ARA
Ø CCB (except verapamil) plus betablocker
Alpha blockersmay be used with any of the other classesbut are
usually reserved for third-line therapy unless specificallyindicated for
another reason. A 3-drug combinationis often required, especially in severe
hypertension. Inpatients who maintain an elevated diastolic blood
pressuredespite triple therapy the possibility of secondary hypertensionshould
be considered, although factors such as non-compliance, NSAID use, or alcohol
abuse may contributeto resistance[83,84].
Other classesof antihypertensive drugs that are sometimesused
include: centrally acting drugs such as clonidine,methyldopa, and the less
sedating moxonidine; direct-actingvasodilators such as hydralazine and
minoxidil; the aldosteroneantagonist, eplerenone; and the
DRI,aliskiren[3]. Endopeptidase inhibitors and
endothelinantagonists are among various drug groups thatare under
investigation.
It has been standard teachingthat drug treatment for
hypertension is continued indefinitely,but there have been some reports of
successfulwithdrawal in selected patients[85,86]. If this is
attempted,blood pressure must be closely monitored and lifestylemeasures should
be continued indefinitely[40,81].
G. ADHERENCE TO ANTIHYPERTENSIVE THERAPY
The mainobjective of hypertension management is to achieve BP
control through changes in lifestyle andappropriate therapeutic
measures[1,3]. In the recent years,a growing number of
patients seem to present resistanceto the antihypertensive
treatment[87]. Non-adherence has important economic
implications: itdecreases the cost-effectiveness of interventions, leading
topoor clinical results with increased costs for public
health[88].
Different methods to measure therapeutic adherence
areavailable; all have favourable and unfavourable aspects andthere currently
is no gold standard[10]. These methods canbe classified as
direct or indirect: interviews and questionnairesadministered to patients (one
of the most used isMorisky's scale), diaries, pill count, electronic
monitoringof orally administered drugs, rates of prescriptions'
refillingthrough pharmacies' databases and direct dosage ofdrug levels in
biological fluids[10].At the present time therapeutic drug
monitoring (TDM)is available for most antihypertensive drugs and severalstudies
have demonstrated its efficacy in the evaluation
ofadherence[89,90].
1. Definition and Forms of Non Adherence
Therapeutic adherence describes the extent to which patients
actively take medications as prescribed by their health care providers based on
a therapeutic alliance or contract established between them; it differs from
the term compliance, withwhich it is often confused[10]. The
term compliance suggests apassive attitude when the patient follows the
physician'sinstructions and treatment plan, without a real
therapeuticalliance[10].In any case, these two terms do not
allow to differentiatepatients who systematically fail to follow the
recommendationsfrom those who occasionally forget a pill or reducethe dose of
the drug[91].
Several conditions could affect therapeutic adherence:type of
prescribed therapy, patient socio-cultural level,frequency of clinical
controls[92]. The WHO hasidentified five different
conditions[23] correlated with pooradherence: social and
economic factors, condition-relatedfactors, therapy-related factors,
patient-related factors andhealth care system/health care team-related factors.
Moreover,frequently patients start the prescribed therapy, butadherence is
progressively reduced because they do notpersist[23].
2. Methods for assessing drug adherence
Different methods to measure therapeutic adherence
areavailable. Indirect methods are less invasive andless expensive. Indirect
methods for evaluating drug adherence include: patient interview, diaries,
questionnaires,pill count, review of prescriptions, electronic
monitoring[15,21].Conversely, direct methods are more
invasive, expensiveand include the direct observation of the patient duringthe
administration of therapy and the measurement of thedrug or of its metabolites
in blood or urine[93]. Nonetheless, only a limited number of
drugs can be monitored in this way because the bioavailability and
completenessof absorption of various drugs, as well as the rate of
metabolismand excretion, are factors that make it difficult tocorrelate drug
concentrations in blood or urine with adherence[15].
In clinical practice, each method has advantages
anddisadvantages and not all can be easily used in all settings;it is often not
possible to accurately determine the realdegree of adherence.
2.1 Patient Interview[15,21,94]
The patient interview is one of the simplest and lessexpensive
methods, but its efficacy is strongly influenced bythe ability of the
interviewer and by the way in which thequestions are asked; it also heavily
relies on a strongdoctor-patient relationship. Interviews may allow a
pharmacist to show concern for the patient andprovide immediate feedback.
Typical questions include askingthe patient to report the name, the dosage and
the timeof drug intake. Alternatively, the doctor may ask the patienthow often
they forget to take the pills during a week or amonth; according to the answers
the physician can theninfer the degree of adherence.The patient interview can
also be targeted to encouragebehavioural changes and to improve therapeutic
adherence.
A drawback of this method isthat it can overestimate
adherence, and its accuracy dependson the patient's cognitive abilities and the
honesty of replies,as well as the interviewer's correct interpretation of
responses.
2.2 Questionnaires[94,95]
The questionnaires are simple and economical methods
toevaluate adherence. They are usually composed of a limitednumber of questions
that the patient is asked to answer.A potential disadvantage is represented by
the difficultysome subjects may have understanding the questions incase of low
level of education.One of the most frequently used questionnaire is theMorisky
8 items MMAS-8 (Eight-Item Morisky MedicationAdherence Scale), which has a
higher specificity(93%) compared to the original 4-item questionnaire.The
MMAS-8 consists of seven binary questions (YES/NO) and one last multiple choice
question. A clearlimitation of this instrument is represented by patients
whomight answer the questions untruthfully. Similarly to thepatient interview,
questionnaires are useful to evaluateunintentional poor adherence.
2.3 Pill Count
Counting pills is a simple and cost-effectiveness method
toevaluate therapeutic adherence, but it is characterized byseveral
limitations[94]. Among these, the most relevantlimitation is
represented by the fact that patients canmislead the doctor, throwing away the
pills before the visit.Furthermore, this method does not provide
accurateinformation on daily adherence[10].The accuracy of the
pill count method is adequate when compliance is excellent because there is
nothing to return; however, in cases of low compliance, the pill count is not
accurate.
An effective but at the same time more complex andexpensive
method is electronic monitoring, in which thepill count is performed
automatically and continuously by adevice at the patients'
home[96].
2.4 Electronic Monitoring[94,97]
There are different electronic monitoring systems, usuallyvery
expensive and invasive. However, in view of theirhigh efficacy they can be
considered as the gold standardfor assessing drug adherence.One of the less
invasive options is the medication events monitoring system (MEMS), which uses
a device to recordthe time and the date in which medications are taken fromthe
box. In the last years, a more invasive system was validated: the ingestible
sensor technology. In thiscase the sensor is inside the pill, so it becomes
possible toaccurately document each time a pill is ingested.
2.5 Therapeutic Drug Monitoring (TDM)
The most accurate direct method for evaluating
therapeuticadherence is the measurement of the drug concentration (orthe
concentration of its metabolites) in body fluids (bloodor
urine)[94]. For this purpose, liquid
chromatography-massspectrometry analysis can be used[93].In
the recent years, several studies used TDM to evaluatetherapeutic adherence,
especially in patients withsuspected resistant
hypertension[89,90]. Chung et al.[98]have
recently demonstrated that TDM is a cost-effectivemethod to assess adherence in
the workup of resistanthypertension, independently by sex and age. TDM
wouldallow a substantial economic advantage when comparedwith previous
cost-effectiveness analyses of invasive proceduresfor the treatment of
resistant hypertension[99,100].
TDM, however, has some limitations: it provides resultswithout
giving information about the causes of non-adherence;it is very intrusive for
the patient; it can induce thephenomenon of white-coat adherence;
antihypertensivedrugs can present an altered metabolism when taken withother
drugs. An ethical problem should also be considered:such measurements need to
be done with the informedconsent of patients and thus tend to induce
white-coatadherence[94]. Despite these limitations, TDM, used
inselected cases, may provide a way to decrease health costs, by reducing the
number of visits in patients who intentionallydo not take drugs and by
identifying those patientswho would undergo unnecessary and sometimes
invasiveprocedures.
3. Improving Therapeutic Adherence[21,101]
Properly identify patients who do not take prescribedtherapy
has important consequences, such as execution ofunnecessary medical visits or
diagnostic tests, as well asscreening evaluation for secondary forms of
hypertension.For this reason it is important to improve therapeuticadherence in
all patients with hypertension, mostly in thosewith difficult to treat or
resistant hypertension. Although itis a difficult task, physician should help
individual patientto get better therapeutic compliance.
There are different strategies for improving long
termtherapeutic adherence: simplifying medical regime withfixed associations of
drugs when available, giving patientsinstructional material, counselling about
therapy, remindingfor medications and appointments, cuing medications todaily
events and explicitly acknowledging patient's effortto adhere.Therefore,
treating physician should establish a goodrelationship with each individual
patient to address andresolve poor therapeutic adherence.
4. Reasons for poor therapeutic adherence
v Non-African countries
In a cross-sectional study carried out by Lin et al. in 1995
in Tainan City, the medication adherence rate found was 57.6%. Subjects taking
80% or more of their prescribed medicines were considered
adherent[102]. The factors associated significantly with poor
adherence included: more than once daily dose frequency, no health check-up in
the previous year, disbelief in the efficacy of antihypertensives, and presence
of adverse drug reactions in the past 6 months.
In a cross-sectional study by Hashmi et al. in 2005 in
Pakistan, 77% of their cases were adherent. Univariate analyses showed that
decreasing age, poor awareness and decreasing number of pills prescribed
significantly promoted poor adherence[103].
In Bangladesh, Hussain et al. found in 2006 that 85% of the
study population were non-adherent to treatment. The reasons pointed out were
low levels of education, low family income, duration of diagnosis, insufficient
knowledge of the disease, lack of accompanying person to go to the
physician/hospital, and deficiencies in information from the service
provider[104].
In a cohort study carried out in Italy involving 18,806 newly
diagnosed hypertensive patients =35 years of age, Mazzaglia et al. in 2009
found varying adherence rates. 6 months after index diagnosis, the authors
found rates of 8.1%, 40.5%, and 51.4% corresponding to high, intermediate, and
low adherence levels, respectively. The authors also found thatthe risk of
being a poor adherer increased in the absence of concurrent
treatment[105].
In a descriptive exploratory study conducted by Demoner et al.
in 2011 in Brazil, 64% of patients in the study were nonadherent to
antihypertensive therapy. Adherence level was assessed using the Morisky-Green
Test. Poor adherence was significantly associated with participants who were:
in the youngest age group, working, lack of understanding of the health team
recommendations and presenting with overweight or
obesity[106].The younger patients (18-40 years) presented
lowerlevels of adherence compared to those in older agegroups. This may be
related to the fact that HTN is asilent disease and, thus, leads to a certain
nonchalance inyounger individuals regarding the control of the disease,who only
give importance to adequate treatment whenthere is a worsening of symptoms,
increasing risks ofserious complications and mortality for stroke and MI.
In a cross-sectional study carried out in 2014 in Iran,
Behnood-Rod et al. found that about half of the sample population (49.6%)
showed low adherence (8-item Morisky Medication Adherence Scale <6). In
addition the authors also found that overweight/obesity, previous history of
admission to emergency services due to hypertensive crisis, and getting
medication directly from drugstore without refill prescription in hand were
factors recognized to have statistically significant association with the
8-item Morisky Medication Adherence Scale score[107].
In a retrospective cohort study including 5025 Swedish adult
patients in 2015, Hedna et al. found that non-adherence to any antihypertensive
medication was higher among persons < 65 years (17.5%) and with the lowest
income (12.8%). Also the authors found that, non-adherence to the full AHT
regimen was higher among new users (44.2%), persons using specialized
healthcare (38.3%) and having multiple antihypertensive medications (54.3%).
Finally, the authors noted that non-adherence to any antihypertensive
medication a month prior to healthcare visit wasassociated with elevated
BP[108].
In cross-sectional correlational study by Lo et al. in Hong
Kong in 2016, more than half of the respondents (55.9%) acknowledged some
degree of medication nonadherence. Older age, living alone, and perception
related to treatment control were independently associated with increased odds
of medication non-adherence[109].
v African countries
In a cross sectional study carried out in Northwest Ethiopia
in 2011, Ambaw et al. found that more than half (64.6%) of the study
participants were found to be adherent to their treatment. Male gender,
insufficient knowledge about hypertension and its treatment, distance from the
hospital and presence of comorbidity were found to be significantly associated
with poor treatment adherence[7].
In 2013, Okwuonu et al. found in a cross-sectional study
carried out in Nigeria that BP control was optimal in 33%, good knowledge of
hypertension was found in 52% and only 31.8% were adherent to prescribed
medications. The authors also added that the duration ofhypertension from time
of diagnosis, systolic and diastolic blood pressures andtotal number of pills
swallowed per time were found to independently correlatewith medication
adherence, albeit negatively[110].
In a multicenter cross-sectional study conducted in 2013 by
Boima et al., medication non-adherence was found in 66.7% of the study
population. Medication non-adherence showed correlation with depression,
concern about medications, and knowledge of hypertension. Adherence was
associated with formal education and use of herbal preparation. Poor BP control
was observed in 69.7% and there was significant association between medication
non-adherence and poor BP control[111].
v In Cameroon
Tufon et al. found in a cross-sectional study carried out at
the Mankon Sub-Divisional Health Center in 2014 that level of adherence was
found to be low (80.0%) with smoking (85%) and alcohol intake (55%) identified
as associated factors. Moderate level of knowledge (77.5%) was found as opposed
to a high level of adherence (80.0%) and the authors found no significant
relationship between the level of knowledge and level of
adherence[18].
Essomba et al. reported in 2015 in a cross-sectional and
analytical study, that 26.2% of their study population had good adherence to
antihypertensive treatment. At the same time, 25.7% were bad adherers. Reasons
for non-adherence included: forgetfulness, medication cost and poor knowledge
of the disease[19].
Akoko et al. in 2015 reported that antihypertensive compliance
rate was 43.9% in their cross-sectional study. Independent predictors of
noncompliance were forgetfulness, lack of motivation due to the incurable
nature of the disease, and lack of symptoms of the
disease[20].
Mbouemboue et al. reported in 2016 that, 12.9% of patients
enrolled in the study in the Medico-Social Centre of the National Social
Insurance Fund in Garouafollowed up their treatment correctly, 52.9% had minor
observance problems, and 34.3% had a poor therapeutic adherence to
antihypertensive drugs. Therapeutic adherence was evaluated on the basis of the
Girerd X observance test. The determining factors of poor adherence were the
presence of complications of high BP, the presence of a handicap, and a low
level of education[16].
CHAPTER III: MATERIALS AND
METHOD
1. STUDY DESIGN
This was a cross-sectional analytic study.
2. DESCRIPTION OF THE STUDY SITE
This study was conducted at the external consultation service
of the cardiology unit of the Yaounde General Hospital (YGH) which is located
in Yaounde, the capital city of Cameroon.YGH serves as a teaching centre, and
is a reference hospital for other hospitals in the Centre region.
YGH is a state-owned hospital made up of several units:
internal medicine, surgery,
obstetrics, gynaecology and paediatrics. It covers an area of
20,301 square metres and as of 2001 had 302 beds. Inhabitants from Yaounde and
beyond come to this reference health institution to seek for general and
specialized health services.
3. STUDY PERIOD
This study was carried out over a period of seven months
(November 2017 - May 2018).
4. SAMPLING
4.1 Study population
Hypertensive patients receivingantihypertensive treatment as
outpatients at the YGH.
4.2 Inclusion criteria
Ø Hypertensive patients aged 18 years and above;
Ø Outpatients diagnosed with HBP and on
antihypertensive drug treatment for at least 6 months prior to recruitment
period;
Ø Patients who consent to be enrolled in the study.
4.3 Non-inclusion criteria
Outpatients with hypertension:
Ø andwith mental impairment or psychiatric disease;
Ø with difficulty in communication and without a
translator;
Ø who gave incomplete information necessary for the
study;
Ø unable or unwilling to give informed consent.
4.4 Sample size
Cochran'sformula[112],   , was used to estimatethe sample size. , was used to estimatethe sample size.
The following assumptions were made:previous data indicated an
adherence rate of 12.9% in Garoua[16]. So proportion was taken
as 12.9%(p = 0.129), 95% confidence interval, and 5% margin of error(d = 0.05).
Computing into the above formula:

n = Minimum sample size required
p= Antihypertensive adherence rate
d= Error margin of 5%
Z1-á/22 =95%
confidence interval (value type=1.96)
Therefore, from the above formula a minimum sample size of 173
patients was required for the study.
5. MATERIALS
5.1 Materials for data collection
Ø Patientmedical records.
Ø Case report forms (CRFs) for data collection.
Ø Ballpoint ink-pens, pencils, and erasers.
5.2 Materials for data analysis
Ø A laptop with Microsoft®Office Tools
2013 for data entry and Epi-infoTMsoftware Version 3.5.4 for data
analysis.
Ø An 8 GB flash disk.
5.3 Materials for Blood Pressure
Measurement
Ø A calibrated electronic sphygmomanometer (Model:
LD-578)
Ø A stethoscope
6. DATA COLLECTION PROCEDURE
Administrative and ethical approvals
In accordance with research ethics, ethical clearance was
obtained from the Institutional Review Board of the Faculty of Medicine and
Biomedical Sciences of the University of Yaounde I(APPENDIX
1A), as well as authorization from the Director of the YGH before the
recruitment of patients for the study (APPENDIX 1B). The study
was explained to the patients and informed consent by signature was obtained
prior to their enrolment into the study (APPENDIX 2). During
the study, the case report forms (APPENDIX 3) were kept secret
by the investigator from people not involved in the study, in order to respect
patient confidentiality.
Approach with the participants
The patients admitted into this study were selected
consecutively at the external consultation service of the cardiology unit.
Patients that met our inclusion criteria were selected during consultations and
interviewed immediately after. After obtaining their written consent, we
proceeded by measuring their resting BP. Two sitting BP measurements were taken
on both arms with a pretested electronic sphygmomanometer approximately 2
minutes apart. Another 2 minutes later, a third measurement was taken on the
arm with the highest BP reading. Then an average of the last two readings was
eventually used to determine the BP level during the visit. After recording the
BP reading, we proceeded with an interview of the patients in order to fill the
pretested questionnaires. BP measurements and interview were carried out in
private in a consultation box. The 2014 Evidence-Based Guideline for the
Management of High Blood Pressure in Adults[113] was used to
evaluate the level of control of patient BP:
v Hypertensive patients aged 60 years and above were
considered to have a controlled hypertension if their average BP reading
was<150/90 mmHgduring the last 3 months and if they presented with no
diabetes nor chronic kidney disease.
v Hypertensive patients aged 60 years and above were equally
considered to have a controlled hypertension if their average BP reading
was<140/90 mmHg during the last 3 monthsif they presented with diabetes or
chronic kidney disease.
v Also, patients aged under 60 were considered to have a
controlled hypertension if their average BP reading was<140/90 mmHgduring
the last 3 months and if they presented with or without other comorbidities
(diabetes and chronic kidney disease).
At the end, the questionnaires were cautiously stored prior to
data analysis.
The variables to be investigated consisted of:
Ø Sociodemographic data (independent
variables): Age, sex, zone of residence, marital status, trip duration
to the hospital, level of education, and profession.
Ø Socioeconomic data (independent
variables):Socioeconomic status (which is an adapted classification
from theRevised Kuppuswamy's socio-economic status scale- January
2015[114](see APPENDIX 3) where the projected
family income was estimated from the Gross National Income (GNI) per capital;
health insurance; monthly drug costs. A score of <5 was considered low;
between 5 and 10 was considered middle; and >10 was considered high
socioeconomic status.
Ø Clinical characteristics of
respondents(independent variables):Comorbidities present (if any);
blood pressure readings; handicap present (if any).
Classification of BP:SBP <120mmHg and DBP
<80mmHg was considered optimal; SBP [120-129]mmHg and/or DBP [80-84]mmHg was
considered normal; SBP [130-139]mmHg and/or DBP [85-89]mmHg was considered High
Normal; SBP [140-159]mmHg and/or DBP [90-99]mmHg was considered Grade I
hypertension; SBP [160-179]mmHg and/or DBP [100-109]mmHg was considered Grade
II hypertension; SBP=180mmHg and/or DBP =110mmHg was considered Grade III
hypertension; SBP =140mmHg and DBP <90mmHg was considered isolated systolic
hypertension.
Definition of heart failure:Inability of the
heart to ensure blood flow necessary for the metabolic and functional needs of
body organs. Clinical signs include edema, tachycardia, and rales with low
ejection fraction (EF<43%).
Diagnostic criteria for
hypercholesterolemia:
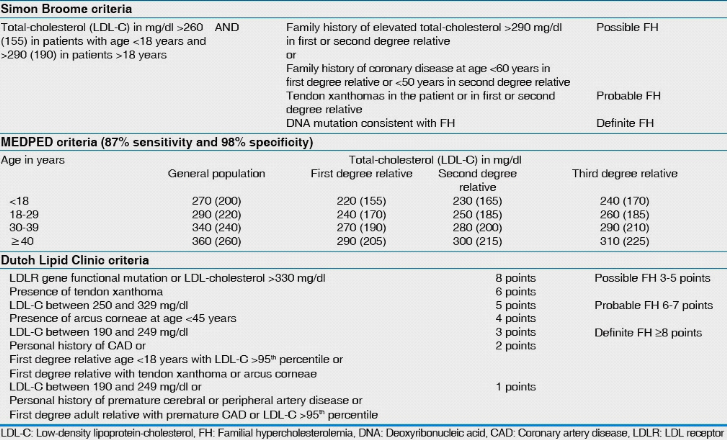
Figure 7: Dutch Lipid
Clinic criteria
Definition of obesity:BMI >24.9
kg/m2.
Diagnostic criteria for diabetes: A1C =6.5%
or Fasting Plasma Glucose =126 mg/dl (7.0 mmol/l) or 2-h plasma glucose =200
mg/dl (11.1 mmol/l) during an Oral Glucose Tolerance Test or in a patient with
classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma
glucose =200 mg/dl (11.1 mmol/l).
Definition of gout:Inflammatory
microcrystalline arthropathy associated with intense pain and related to a
disruption of the metabolism ofuric acid.Hyperuricemia is generally above 390
umol/L (6.5 mg/dL).
Diagnostic criteria for arthritis:Prolonged
morning stiffness, swollen joints, and painful/inflamed joints.
Diagnostic criteria for gastritis: Nausea,
abdominal pain, bloating, vomiting, indigestion, and burning feeling in the
epigastric region.
Diagnostic criteria for hyperthyroidism:
Nervousness, mood swings, muscle weakness, heat intolerance, insomnia,
hand tremors, tachycardia, diarrhea, weight loss, enlarged thyroid gland, and
elevated thyroid stimulating hormone, free thyroxine and total triiodothyronine
levels.
Definition of epilepsy: Presence or history
of recurrent convulsions which are involuntary, violent, and spasmodic or
prolonged contraction of skeletal muscles.
Definition of anemia: Decrease in hemoglobin
per unit of blood volume below physiological values i.e. 13 g / dL in men; 12 g
/ dL in women and children.
Diagnostic criteria for benign prostate
hypertrophy: Presence of enlarged prostate, high prostate specific
antigen levels, polyuria, weak stream and/or urinary incontinence.
Diagnostic criteria for depression: Presence
of psychological symptoms (low mood, low self-esteem, feeling irritable, no
interest in things, anxiety, suicidal thoughts); and physical symptoms (changes
in weight, constipation, unexplained pains, loss of libido, changes in
menstrual cycle).
Definition of glaucoma: Intraocular pressure
above an upper normal value of 21 mmHg.
Diagnostic criteria for hemorrhoids: Presence
of bleeding with or without defecation, mucous discharge, pruritus, incomplete
evacuation, distal rectal mass upon digital exam, and presence of fissures
after anoscopy.
Diagnostic criteria for deep venous thrombosis:
Presence of pain, swelling and tenderness in legs, warm skin in the
area of the clot upon palpation, positive D-dimer test, detection of clots with
Doppler ultrasound.
Definition of physical handicap: Presence of
physical defects, including upper or lower limb loss or poor manual
dexterity.
Definition of sensory handicap: Presence of
visual impairment or blindness, hearing loss or deafness.
Ø Therapeutic characteristics of
respondents(independent variables): Type of therapy; molecule(s)
prescribed;Drugs prescribed (pioneer or generic); Antihypertensive drug groups
prescribed; number of drugs used per day; Dosage schedule; Presence of side
effects (if any); Duration onantihypertensive treatment.
Ø Adherence profile (dependent
variable):The Eight-Item Medication Adherence Scale (Table VI) was
used to assess therapeutic adherence[95].
We assessed the adherence level of the study population by
using the validated MMAS-8. The scale is based on patients`
self-response.Patients with a score of 8 on the scale were termed highly
adherent, medium adherers were those with a score of 6 to <8, and those
classified as lowadherers were those with a score of <6.This medication
adherence scale has the advantage of beingrelatively simple and practical to
use in clinical settings. The instrument was used to identify patients with
adherence problems, and could also be used to monitor adherence over the course
of the treatment. One important feature of the scale is that treatment-related
attitudinal and behavioral problems thatthe patient may be facing can be
immediately identified and health care providers may provide reinforcement and
advice such that the patient can take positive steps early on to address these
issues. Patients were considered to have a poor adherence if they had <8 and
good adherence if they scored 8 on the MMAS-8 (Table VII).
Ø Patient knowledge (independent
variable)
Data concerning patients' knowledge of hypertension (i.e.
causes, treatment, and complications) was also collected on the pretested
questionnaires (APPENDIX 3). Knowledge scores for individuals
were calculated and summed up to give a total knowledge score. The scoring
range isfrom 0 (minimum) to 16 (maximum). A cut-off score of <8 was
considered as poor knowledge, ascore of [8-12] was considered knowledgeable and
a score of [13-16] was considered good knowledge.
Table VI: The 8-Item Medication Adherence
Scale[95]
|
ITEM
|
CORRECTED ITEM-TO-TOTAL CORRELATION
|
|
1. Do you sometimes forget to take your
high blood pressure
pills?
|
.4639
|
|
2. Over the past 2 weeks, were there any
days when you did
not take your high
blood pressure medicine?
|
.5108
|
|
3. Have you ever cut back or stopped
taking your medication
without telling
your doctor because you felt worse
when you took it?
|
.4277
|
|
4. When you travel or leave home, do you
sometimes forget
to bring along your
medications?
|
.4095
|
|
5. Did you take your high blood pressure
medicine
yesterday?
|
.3038
|
|
6. When you feel like your blood pressure
is under control,
do you sometimes
stop taking your medicine?
|
.5044
|
|
7. Taking medication everyday is a real
inconvenience for
some people. Do you
ever feel hassled about sticking to your
blood
pressure treatment plan?
|
.4009
|
|
8. How often do you have difficulty
remembering to take all
your blood
pressure medication?
|
.5896
|
|
á Reliability, .83.
|
|
Table VII: Cut-offs for
MMAS-8
|
Cut-off score
|
Adherence status
|
|
8
|
High adherers
|
Good adherence
|
|
|
|
|
[6-8[
|
Medium adherers
|
Poor adherence
|
|
<6
|
Low adherers
|
7. STATISTICAL ANALYSIS
Data entry and analysis was undertaken using the statistical
software Epi Info version 3.5.4. Data cleaning was performed to check for
accuracy, consistency and that there were no missed values during entry.
Frequencies, proportions and summary statistics were equally generated to
describe the study population in relation to the relevant variables.Bivariate
analysis using the chi2test was carried out to assess associations of each
independent variable with thedependent variable. Variables with P-value<
0.05 in bivariate analysis were selected as candidate variables for
multivariate analysis with logistic regression. Odds ratio and 95% confidence
interval were used to identify the presence andstrength of association.
Statistical significance was considered at P-value < 0.05.
8. HUMAN RESOURCES
Ø Supervisor: Pr MENANGA Alain Patrick
Ø Co-supervisor: Dr. TEMBE Estella épse FOKUNANG
Ø Investigator: CHIABI Roland MUNTOH
Ø Collaborators: Medical and paramedical personnel
Ø A statistician
CHAPTER IV: RESULTS
IV.1 STUDY FLOW PROFILE
In this study, 181 potential participants were identified
during consultations. Of the 6 patients not included 3 did not have time to
participate in the study and 3 gave incomplete information. 175 patients were
finally retained for the study as they complied with the stated inclusion
criteria.
Figure 8 below illustrates a flow diagram of the recruitment
process.
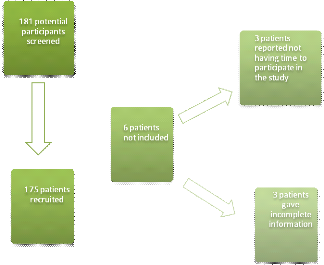
Figure 8: Participant flow
chart
I- SOCIODEMOGRAPHIC AND SOCIOECONOMIC CHARACTERISTICS OF
THE STUDY POPULATION
Table VIII shows the sociodemographic characteristics of study
participants.
Of the 175 patients recruited into the study, 54.90% were men
and 45.10% were women with a sex ratio of 1.2.
The mean age of the study participants was 60.1 #177; 11.1
years with extremes from 33 to 88 years and with the age group =60 years being
the most represented (48%; n =48).
The majority of the participants lived in an urban setting
(88.60%), while 11.40% of them lived in rural communities.
Among the 175 participants, 51.43% had a non-liberal
profession and 21.14% were unemployed. The non-liberal class was represented in
majority by public servants.
Of the 175 participants, 66.30% of participants lived as a
couple either legally married or not while 33.7% were single (either divorced,
never married or widowed).
Most participants in our study (40%) had a higher education.
2.3% never went to a formal system of education.
Among the 175 participants, 84.60% spent less than 1 hour to
reach the YGH. The mean trip duration was 38.6 #177; 30.8 minutes with extremes
between 5 minutes and 3 hours.
Three sociodemographic factors were found to be significantly
associated with poor therapeutic adherence: single marital status (OR = 4.66;
CI95 =2.07 - 11.28 ; p <0.001); 1st cycle
secondary education (OR = 3.03; CI95 =1.22 - 8.42 ; p
<0.001); and more than 1 hour trip duration (OR = 7.39; CI95
=1.93 - 47.51; p <0.001).
Urban place of residence (OR = 0; CI95 =0 -
0.29 ; p <0.001); living as a couple (OR = 0.21; CI95 =
0.09 - 0.48 ; p <0.001) and <1 hour trip duration (OR = 0.14;
CI95 =0.02 - 0.52; p <0.001) were significantly associated with
good adherence.
Table VIII: Sociodemographic
characteristics of the study population
|
Poor adherence
|
Good adherence
|
Total
|
P-value*
|
PA**
|
|
Sociodemographic variables
|
n (%)
|
n (%)
|
n (%)
|
|
|
|
Gender
|
|
|
|
|
|
|
Male
|
66 (68.8)
|
30 (31.3)
|
96 (54.9)
|
0.400
|
|
|
Female
|
52 (65.8)
|
27 (34.2)
|
79 (45.1)
|
0.400
|
|
|
Age (years)
|
|
|
|
|
|
|
<40
|
4 (80)
|
1 (20)
|
5 (2.9)
|
0.470
|
|
|
[40-50[
|
18 (75)
|
6 (25)
|
24 (13.7)
|
0.270
|
|
|
[50-60[
|
43 (70.5)
|
18 (29.5)
|
61 (34.9)
|
0.320
|
|
|
=60
|
53 (62.4)
|
32 (37.6)
|
85 (48.6)
|
0.110
|
|
|
Place of residence
|
|
|
|
|
|
|
Urban
|
98 (63.2)
|
57 (36.8)
|
155 (88.6)
|
<0.001
|
|
|
Rural
|
20 (100)
|
0 (0)
|
20 (11.4)
|
0.000
|
|
|
Profession
|
|
|
|
|
|
|
Liberal
|
28 (58.3)
|
20 (41.7)
|
48 (27.4)
|
0.080
|
|
|
Non-Liberal
|
61 (67.8)
|
29 (32.2)
|
90 (51.4)
|
0.520
|
|
|
Unemployed
|
29 (78.4)
|
8 (21.6)
|
37 (21.1)
|
0.080
|
|
|
Marital status
|
|
|
|
|
|
|
Single
|
51 (86.4)
|
8 (13.6)
|
59 (33.7)
|
<0.001
|
0.0003
|
|
Couple
|
67 (57.8)
|
49 (42.2)
|
116 (66.3)
|
<0.001
|
|
|
Level of education
|
|
|
|
|
|
|
Never gone to school
|
3 (75)
|
1 (25)
|
4 (2.3)
|
0.610
|
|
|
Primary
|
19 (70.4)
|
8 (29.6)
|
27 (15.4)
|
0.460
|
|
|
Secondary-1st cycle
|
31 (83.8)
|
6 (16.2)
|
37 (21.1)
|
0.010
|
0.0209
|
|
Secondary-2nd cycle
|
22 (59.5)
|
15 (40.5)
|
37 (21.1)
|
0.170
|
|
|
Higher education
|
43 (61.4)
|
27 (38.6)
|
70 (40)
|
0.110
|
|
|
Trip duration (hour)
|
|
|
|
|
|
|
<1
|
93 (62.8)
|
55 (37.2)
|
148 (84.6)
|
<0.001
|
|
|
=1
|
25 (92.6)
|
2 (7.4)
|
27 (15.4)
|
<0.001
|
0.008
|
*p-value from Chi-square test; **PA is p-value
adjusted for significant factors obtained from logistic regression analysis
using variables with P < 0.05 in bivariate analysis as candidate
variables.
Figure 9 shows the distribution of participants according to
socioeconomic status. The high socioeconomic status group was greatly
represented (60%) in our study followed middle socioeconomic status group
(39.40%).Middle socioeconomic status was found to be significantly associated
to poor therapeutic adherence (OR = 2.68; CI95 = 1.33-5.53; p <
0.001).
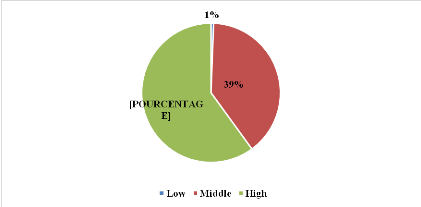
Figure 9: Distribution
according to socioeconomic status
Figure 10 shows the distribution of participants according to
possession of health insurance. Only 11.00% of our study population had a
health insurance.
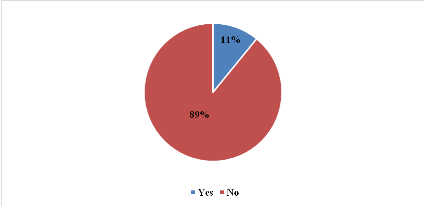
Figure 10:Distribution
according to possession of health insurance
II- CLINICAL AND THERAPEUTIC CHARACTERISTICS OF THE STUDY
POPULATION
Figure 11 shows the BP distribution of the study participants.
The High Normal BP group was the most represented (n=43; 24.60%). Only 4.60%
had a Grade III hypertension.
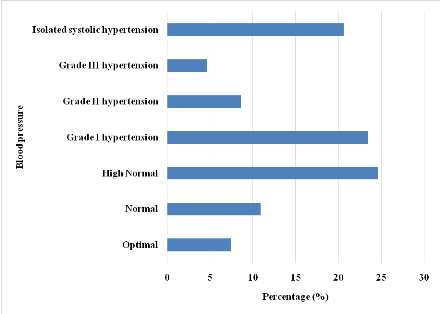
Figure 11: Blood pressure
distribution of the study population on enrolment
Figure 12 shows the distribution of participants according to
BP status. 57.70% of the study population had a controlled BP and 42.30% were
uncontrolled.
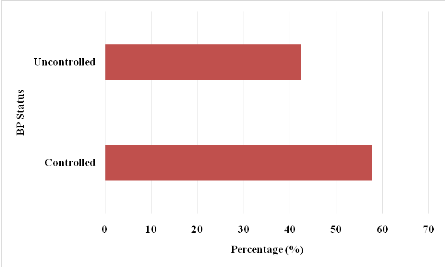
Figure 12: Blood pressure
status distribution of the study population
Figure 13 illustrates the distribution of comorbidities of the
study population. The most frequently associated pathology to HBP was heart
failure (24.57%) followed by hypercholesterolemia (20.00%).
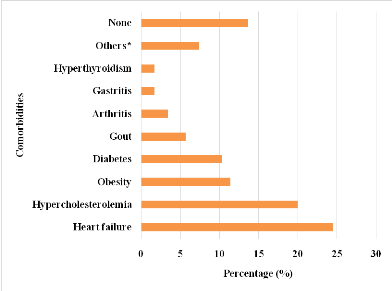
*Other comorbidities encountered in the study included :
gout, arthritis, gastritis, hyperthyroidism, epilepsy, anemia, asthma, benign
prostate hypertrophy, depression, glaucoma, haemorrhoids, and deep venous
thrombosis
Figure 13: Distribution of
comorbidities of the study population
Figure 14 shows the distribution of participants according to
type of handicap.32 participants had a form of handicap. 16.57% of the study
population had a motor handicap and 1.71% had a sensory handicap. Presence of
handicap was found to be significantly associated to poor therapeutic adherence
(OR = 4.12; CI95 = 1.45-14.34; p < 0.001).
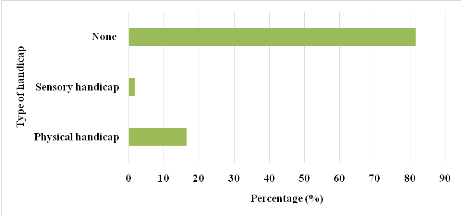
Figure 14: Distribution
according to type of handicap
Table IX shows the different classes screened in the study.
Calcium channel blockers was the most encountered (31.90%) monotherapy drug
class in our study. ACE inhibitors/thiazide diuretics was the most encountered
fixed-dose combination bitherapy (40.96%). ACE inhibitors/Thiazide
diuretics/CCBs was the most frequent fixed-dose combination tritherapy
encountered (81.80%).
Table IX: Distribution
according to class of antihypertensive used by the study population on
enrolment
|
Fixed-dose therapies
|
Number
|
Percentage (%)
|
|
Monotherapy
|
|
|
|
CCBs*
|
69
|
31.90
|
|
BBs**
|
40
|
18.50
|
|
Loop diuretics
|
39
|
18.10
|
|
ACE*** inhibitors
|
29
|
13.40
|
|
Thiazide diuretics
|
18
|
8.30
|
|
Potassium-sparing diuretics
|
11
|
5.10
|
|
ARA2****
|
7
|
3.20
|
|
Centrally acting antihypertensives
|
3
|
1.40
|
|
Total
|
216
|
100.00
|
|
Bitherapy
|
|
|
|
ACE inhibitors/Thiazide diuretics
|
34
|
40.96
|
|
ACE inhibitors/CCBs
|
18
|
21.69
|
|
ARA2/Thiazide diuretics
|
8
|
9.64
|
|
Thiazide diuretics/CCBs
|
7
|
8.43
|
|
BB/Thiazide diuretics
|
5
|
6.02
|
|
Potassium-sparing diuretics/Thiazide diuretics
|
5
|
6.02
|
|
CCBs/ARA2
|
4
|
4.82
|
|
BB/Thiazide diuretics
|
1
|
1.20
|
|
Thiazide diuretics/Rauwolfia alkaloid
|
1
|
1.20
|
|
Total
|
83
|
100.00
|
|
Tritherapy
|
|
|
|
ACE inhibitors/Thiazide diuretics/CCBs
|
9
|
81.80
|
|
CCBs/ARA2/Thiazide diuretics
|
2
|
18.20
|
|
Total
|
11
|
100.00
|
***ACE: Angiotensin Converting Enzyme; ****ARA2: Angiotensin 2
Receptor Antagonist; **BB: Beta Blocker; *CCB: Calcium Channel Blocker
Table X portrays the therapeutic characteristics of the study
population.
In this study, 81.10% of participants had less than 3
different antihypertensives at the moment of enrolment.
Of the 175 participants, 46.30% had a monthly medication cost
between 10000FCFA and 20000FCFA followed by 33.10% whose monthly drug cost was
<10000FCFA. Only 5.10% had a monthly drug cost of =30000FCFA. The mean
monthly drug cost was 14543 #177; 8613 FCFA with extremes between 800FCFA and
50000FCFA.
Among the 175 participants, 98.30% were on a once daily
medication schedule and 92.60% took their medication(s) in the morning with
breakfast. In this study, 65.70% were on monotherapy and 88.60% were on a
specialty drug. Of the 175 participants, 38.30% experienced side effects with
respect to ongoing treatment.
Among the 175 participants, 55.40% were on treatment for less
than 10 years. Mean duration on treatment was 9.4 #177; 7.3 years with extremes
from 7 months to 36 years.
3 therapeutic variables were found to be significantly
associated with poor adherence; monotherapy (OR = 2.07; CI95 =1.07
- 4; p = 0.020); drug taking in the evening (OR = 2.55; CI95
=1.07-6.62; p = 0.030); presence of side effects (OR = 11.51; CI95
=4.47-34.2; p = 0.000).
<10000FCFA monthly treatment cost was found to be
significantly associated with good therapeutic adherence(OR = 0.5; CI95
=0.26-0.97; p = 0.030).
Table X: Distribution of
therapeutic variables
|
Poor adherence
|
Good adherence
|
Total
|
P-value*
|
PA**
|
|
Therapeutic variables
|
n (%)
|
n (%)
|
n (%)
|
|
|
|
Antihypertensive taken
|
|
|
|
|
<3
|
92 (64.8)
|
50 (35.2)
|
142 (81.1)
|
0.090
|
|
|
=3
|
26 (78.8)
|
7 (21.2)
|
33 (18.9)
|
0.090
|
|
|
Therapy type
|
|
|
|
|
|
|
Monotherapy
|
84 (73)
|
31 (27)
|
115 (65.7)
|
0.020
|
0.0295
|
|
Bitherapy
|
55 (66.3)
|
28 (33.7)
|
83 (47.4)
|
0.440
|
|
|
Tritherapy
|
5 (45.5)
|
6 (54.5)
|
11 (6.3)
|
0.100
|
|
|
Posology
|
|
|
|
|
|
|
Once daily
|
116 (67.4)
|
56 (32.6)
|
172 (98.3)
|
0.700
|
|
|
Twice daily
|
22 (78.6)
|
6 (21.4)
|
28 (16)
|
0.120
|
|
|
Thrice daily
|
1 (100)
|
0 (0)
|
1 (0.6)
|
0.670
|
|
|
Moment the drug was taken
|
|
|
|
|
|
|
Morning
|
109 (67.3)
|
53 (32.7)
|
162 (92.6)
|
0.580
|
|
|
Afternoon
|
6 (60)
|
4 (40)
|
10 (5.7)
|
0.420
|
|
|
Evening
|
31 (81.6)
|
7 (18.4)
|
38 (21.7)
|
0.030
|
0.0399
|
|
Morning, evening
|
22 (81.5)
|
5 (18.5)
|
27 (15.4)
|
0.070
|
|
|
Morning, afternoon, evening
|
1 (100)
|
0 (0)
|
1 (0.6)
|
0.670
|
|
|
Side-effects
|
|
|
|
|
|
|
Yes
|
62 (92.5)
|
5 (7.5)
|
67 (38.3)
|
<0.001
|
<0.001
|
|
No
|
56 (51.9)
|
52 (48.1)
|
108 (61.7)
|
|
|
|
Type of medication taken
|
|
|
|
|
|
|
Specialty
|
106 (68.4)
|
49 (31.6)
|
155 (88.6)
|
0.300
|
|
|
Generic
|
44 (71)
|
18 (29)
|
62 (35.4)
|
0.290
|
|
|
Monthly drug cost (FCFA)
|
|
|
|
|
|
<10000
|
33 (56.9)
|
25 (43.1)
|
58 (33.1)
|
0.030
|
|
[10000-20000[
|
59 (72.8)
|
22 (27.2)
|
81 (46.3)
|
0.100
|
|
[20000-30000[
|
20 (74.1)
|
7 (25.9)
|
27 (15.4)
|
0.290
|
|
=30000
|
6 (66.7)
|
3 (33.3)
|
9 (5.1)
|
0.610
|
|
Duration on treatment (years)
|
|
|
|
|
|
<10
|
66 (68)
|
31 (32)
|
97 (55.4)
|
0.423
|
|
[10-20[
|
37 (71.2)
|
15 (28.8)
|
52 (29.7)
|
0.252
|
|
=20
|
15 (57.7)
|
11 (42.3)
|
26 (14.9)
|
0.132
|
|
*p-value from Chi-square test; **PA is p-value adjusted
for significant factors obtained from logistic regression analysis using
variables with P < 0.05 in bivariate analysis as candidate
variables.
|
III- ASSESSMENT OF ADHERENCE TO ANTIHYPERTENSIVE
TREATMENT
Of the 175 participants, 32.60% were high adherers; 40.60% of
participants were medium adherers; and 26.90% were low adherers. Table XIshows
the adherence profiles of the study population while figure 15 illustrates the
level of adherence.
Table XI: Distribution of
adherence profiles
|
Adherence profile (Morisky score)
|
Number
|
Percentage (%)
|
|
Low adherers
|
47
|
26.90
|
|
Medium adherers
|
71
|
40.60
|
|
High adherers
|
57
|
32.60
|
|
Total
|
175
|
100.00
|
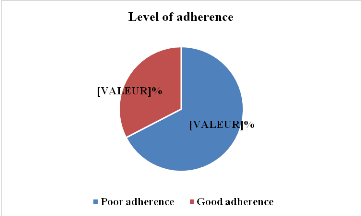
Figure 15: Distribution of
adherence levels
IV- ASSOCIATION OF ADHERENCE WITH BP STATUS
Table XII shows the distribution according to BP status and
good adherence. 36.57% of the study participants who had a poor adherence to
medication equally had an uncontrolled BP. Of the 74 participants having an
uncontrolled BP, 86.49% had poor therapeutic adherence.
Uncontrolled (OR = 5.57; CI95 =2.6-12.48; p =
0.000) BP was found to be significantly associated with poor therapeutic
adherence.
A controlled BP status (OR = 0.18; CI95 =0.08-0.38;
p = 0.000) was found to be significantly associated to good therapeutic
adherence.
Table XII: Distribution
according to blood pressure status and good adherence
|
BP status
|
Good adherence
|
|
Yes (%)
|
No (%)
|
Total (%)
|
|
Controlled
|
47 (26.86)
|
54 (30.86)
|
101 (57.71)
|
|
Uncontrolled
|
10 (5.71)
|
64 (36.57)
|
74 (42.29)
|
|
Total
|
57 (32.57)
|
118 (67.42)
|
175 (100)
|
V- LEVEL OF KNOWLEDGE OF STUDY POPULATION
Figure 16 shows the distribution according to level of
knowledge on hypertension. Of the 175 participants, 54.30% were knowledgeable
about hypertension and 37.7 % had good knowledge.
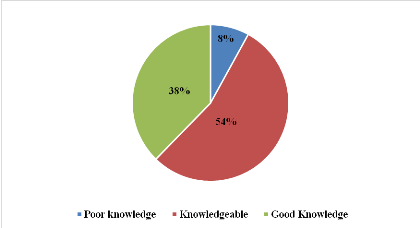
Figure 16: Distribution
according to level knowledge on hypertension
After multivariate analysis with logistic regression 9
predictive factors of poor therapeutic drug adherence were identified (Table
XIII): 1st cycle secondary education(p=0.0209; OR = 3.0287); Single
marital status (p = 0.0003; OR = 4.6623); trip duration of= 1 hour away from
the hospital (p = 0.008; OR = 7.3925); middle socioeconomic status (p = 0.006;
OR = 2.6814);uncontrolled BP status(p = 0; OR = 5.5704); presence of handicap(p
= 0.0117; OR = 4.1222); Monotherapy(p = 0.0295; OR = 2.0721); presence of side
effects(p = 0; OR = 11.5143);and taking medication in the evening (p = 0.0399;
OR = 2.5452).
Table XIII: Predictive factors of poor therapeutic
adherence
|
Variable
|
Odds Ratio
|
C.I. 95%
|
P-Value
|
|
Level of education: Secondary-1st cycle
|
3.0287
|
1.1831-7.7536
|
0.0209
|
|
Marital status: Single
|
4.6623
|
2.0302-10.7068
|
0.0003
|
|
Trip duration: = 1 hour
|
7.3925
|
1.6856-32.4209
|
0.008
|
|
Socioeconomic status: Middle
|
2.6814
|
1.3272-5.4172
|
0.006
|
|
BP status: Uncontrolled
|
5.5704
|
2.5723-12.0626
|
<0.001
|
|
Presence of handicap
|
4.1222
|
1.3706-12.3976
|
0.0117
|
|
Type of therapy: Monotherapy
|
2.0721
|
1.0752-3.9932
|
0.0295
|
|
Presence of side effects
|
11.5143
|
4.2945-30.8719
|
<0.001
|
|
Moment drug is taken: Evening
|
2.5452
|
1.0443-6.2033
|
0.0399
|
CHAPTER V:DISCUSSION
LIMITS AND DIFFICULTIES
Ensuring patient adherence to antihypertensive medications in
order to prevent complications remains a major challenge to public health in
many developing countries. Poor adherence to treatment is the single most
important reason for uncontrolled hypertension, serious complications and
wastage of health care resources [7].
Our main objective was to assess adherence level and its
associated factors to antihypertensive treatment among adult hypertensive
patients followed-up at the YGH. All five specific objectives were achieved by
the end of this study. However some technical difficulties were witnessed which
included: lack of an adequate secluded area at certain times to carry out
interviews privately, incomplete or missing information on patient medical
records, dealing with some patients presenting with comorbidities affecting
their quality of life like stroke, heart failure, gout or diabetic neuropathy
and making participant understand each item of the questionnaires. The study as
a whole has the following limits:
1) The study was carried out in the YGH and so the results
obtained cannot be used to generalize the adherence levels in the Centre
region. More data has to be collected from various hospitals and clinics in
order to bring out a general trend in adherence levels.
2) The research did not investigate adherence levels in
patients suffering from a mental handicap or disease.
3) Refusal of some patients to participate in the study.
v Sociodemographic and socioeconomic
characteristics
Our study sample comprised 175 participants whose average age
was 60.1 #177; 11.1 years. The 60 years and above age group was the most
represented (48%; n = 48). Our results are in line with the previous
literature[1,106-108]. However, in Ethiopia, Ambaw et al.
found in 2012 that the ]40-60[ years age group was predominant at
51.70%[7].Mbouemboue et al. had a similar finding where the
most represented age group was between ]45-65] years old at
57.10%[16]. Nonetheless, what these studies have in common is
that there is a general incremental trend in the prevalence of hypertension in
adults aged 25 and above.
The sex ratio was 1.2 in favor of males (54.90%). Several
authors have reported a similar finding[1,101,102,110].In a
2012 study carried out in Cameroon on 2,120 persons, Dzudie et al. reported
that HBP was more frequent in the male population (50.10%) than in the female
population (44.60%)[28].However other authors reported a
female predominance: Ambaw et al. in 2012 in Ethiopia
at63%[7]; Mbouemboue et al. in 2016 inCameroonat
54.76%[16]; Akoko et al. in 2017 in Cameroon at
55.70%[20]; andEssomba et al. in 2017 in Cameroon
at64.60%[19] and the latter author suggested that a possible
reason for this female predominance is that women take their health issues more
seriously compared to men.
The majority of the participants lived in an urban setting
(88.60%). The YGH is located in the heart of the capital city of Cameroon and
therefore patients who go there for consultations are mostly city
dwellers.Ambaw et al. in 2012 in Ethiopia had a similar finding at
76.60%[7]; and Behnood-Rod et al. in 2016 in Iran had
97.50%[107].
Most participants in our study went through secondary
education (42.29%). Our results were in line with the previous literature
[16,19,20,103,110,111]. This research was undertaken in an
urban setting where basic education is promoted and secondary education
institutions are very much present. Other authors reported lower levels of
education.Tufon et al. in 2014 in Cameroon had 65% of participants whohad
primary level of education possibly because the study site was conducted in a
rural setting[18]; Hussain et al. in 2011 in Bangladesh had
51.70% with primary level of education or below[104].
The majority of our study population (84.60%) spent less than
1 hour to the reach the YGH. The reason for this was that most patients lived
in neighboring quarters. Ambaw et al. in 2012 in Ethiopia had a similar result
where 39.30% spent 30 minutes to reach the hospital and 60.70% spent more than
30 minutes[7].
Only 10.90% of our study population had a health insurance. A
similar result is observed in a study by Mbouemboue et al. in 2016 in Cameroon
who had 8.60%[16]. Thiscould be primarily because of the fact
that health insurance isnot mandatory in the current health-care system, and in
partbecause of the lack of awareness on the benefits of healthinsurance. On the
contrary,Behnood-Rod et al. in 2016 in Iran had 87.80% of participants with
health insurance[107]. A reason for this high record could be
that health insurance is fully integrated into Iranian healthcare systems and
thus easy access to health services.
v Clinical and therapeutic characteristics
Our study revealed that 57.70% of the study population had a
controlled BP. This was higher than what was reported in previous literature.
Mbouemboue et al. in 2016 in Cameroon had 48.57%[16]; Akoko et
al. in 2017 in Cameroon had 42.1%[20]; Behnood et al. in 2016
in Iran had 43.6%[107]; Okwuonu et al. in 2015 in Nigeria had
33%[110]. A reason for the high level of BP control in our
study is that patients are given regular appointments especially upon treatment
initiation in order to appreciate therapeutic efficiency. Physicians comply
with treatment guidelines to change or intensify antihypertensive therapy if BP
remains uncontrolled with pharmacotherapy.
The most frequently associated pathology to HBP was heart
failure at 24.57%. Essomba et al. in 2017 in Cameroon had diabetes at
86.60%[19]; Behnood-Rod et al. in 2016 in Iran had ischaemic
heart disease at 10%[107]; Boima et al. in 2015 in Ghana and
Nigeria had diabetes or renal comorbidities at 27.73%[111];
Hedna et al. in 2015 in Sweden had ischaemic heart disease at 16.4%.
The majority of drugs screened in this study were CCBs
(31.90%) present as fixed-dose monotherapy. Hedna et al. in 2015 in Sweden had
62.10% drugs acting on the renin-angiotensin system in their
study[108]. The reasons for this is that CCBs are first-line
treatment for primary hypertension in patients over the age of 55and black
patients of African[3,68,71,74]. CCBs are also readily
available locally mainly as generics thus facilitating a wider access of
antihypertensives.
The mean monthly drug cost of participants was
14,543FCFA.Mbouemboue et al. in 2016 in Cameroon had a lower average monthly
cost of9,811FCFA per patient per month. The average drug cost was higher in our
study because the majority of drugs prescribed were specialty medications
(88.60%) which are more expensive than their generic counterparts.
v Adherence characteristics
Our study revealed that 32.60% were high adherers; 40.60% of
participants were medium adherers; and 26.90% were low adherers according the
Morisky medication adherence scale.Mbouemboue et al. and Akoko et al.reported
dissimilar figures in their respective studies [16,20].High
adherers were low in a similar study by Behnood-Rod et al. where 49.60% showed
low adherence to antihypertensives, 33.90% had moderate adherence and 16.40%
showed high adherence [107].These figures varied mainly
because of the different methodologies used in assessing adherence.The ultimate
goal of health care intervention is to encourage good adherence of patients to
their antihypertensive drugs. This will have the effect of controlling their BP
thence preventing complications.
v Factors associated with poor adherence
After bivariate analysis 10 variables were found to be
significantly associated with poor adherence (living singly, first cycle
secondary education, trip duration of one hour or more, medium socioeconomic
status, uncontrolled BP status, presence of handicap, monotherapy, taking
medications in the evening, presence of side effects, and knowledgeable about
hypertension). 9 variables persisted after multivariate analysis with logistic
regression (first cycle secondary education, living singly, trip duration of
one hour or more, middle socioeconomic status, uncontrolled BP status, presence
of handicap, monotherapy, presence of side effects, and taking medications in
the evening.
Patients who had a 1st cycle secondary education
were more associated with a poor level of adherence compared to those who had
other educational levels (p=0.0209; OR=3.0287). This was similar
to findings by Mbouemboue et al. in 2016 in
Cameroon[16];Hussain et al. in 2006 in
Bangladesh[104]; and Boima et al. in 2013 in Nigeria and Ghana
also reported insufficient levels of education[111]. Patients
with insufficient background of the disease will have the tendency to neglect
medication adherence and thus be subject to high BP setbacks.
We noted that 66.30% of participants lived as a couple either
legally married or not. Other authors reported similar results
[7,16,18-20,103,106,110,111].Patients who were single were
more associated with a poor level of adherence(p=0.0003; OR=4.6623). Lo et al.
reported in 2016 in China reported a similar finding[109].
Living singly could encourage forgetfulness about drug taking and neglect of
appointments with physicians as opposed to patients living as couples.
Patients who lived 1 hour or more away from the hospital were
more associated with poor therapeutic adherence(p=0.008; OR=7.3925). A similar
finding was gotten from Ambaw et al. in 2012 in Ethiopia[7].
Patients living far away from health centres have the tendency of absenting
from their medical appointments. This can create a breach in patient follow-up,
foster poor adherence and lead to uncontrolled BPs.
Middle socioeconomic status was more associated with a poor
level of adherencecompared to the low and high statuses(p=0.006; OR=2.6814).
Patients in this socioeconomic class usually have difficulties purchasing their
medications which were predominantly specialties and therefore expensive.In
this light, health care providers should promote the prescription of generic
drugs which are affordable and accessible.
Of the 74 participants having an uncontrolled BP, 86.49% had
poor therapeutic adherence.Patients with an uncontrolled BP were more
associated with poor therapeutic adherence than those with a controlled
BP(p<0.001; OR=5.5704). Boima et al. had a similar finding
[111].This association therefore confirms that poor adherence
to antihypertensive medication is responsible for the increasing prevalence of
hypertension.
In our study, 18.29% had a form of handicap of which 16.57%
were physical handicaps. A similar finding was obtained by Mbouemboue et al. in
2016 in Cameroon (18.1%) but with only sensory
handicap[16].Patients with a handicap were more associated
with poor therapeutic adherence compared to those without(p=0.0117; OR=4.1222).
Mbouemboue et al. had a similar finding[16]. Any form of
handicap affects a person's quality of life and also normal medication taking.
Patients with a handicap go through extra challenges in order to correctly take
their medications as prescribed. They therefore need assistance from family and
friends to improve adherence.
Patients who experienced side effects were more associated
with poor therapeutic adherence compared to those who did not experience it
(p<0.0001; odds ratio=11.5143). Lin et al. reported a similar
finding[102]. It is important for physicians to address
medication side effects in patients promptly. This will prevent therapeutic
gaps which are likely to occur in the presence of these side effects. Drug
changes or dosages are therefore imperative in this case.
Patients who took their medications in the evening were more
associated with poor therapeutic adherence compared to those who took their
drugs at other times(p=0.0399; odds ratio=2.5452). Patients are more likely to
forget when told to take drugs in the evening before bedtime. Daily duties
associated with physical and mental stress deter patients from medication
taking thus constituting a hindrance to good adherence.
CHAPTER VI: CONCLUSION AND
RECOMMENDATIONS
VI.1 CONCLUSION
At the end of this study, we could say our different objectives
have been attained and the following points should be retained:
Sex ratio of participants was 1.2 with male predominance of
54.90%. The mean age was 60.1 #177; 11.1 years with extremes from 33 to 88 with
the 60 years and more, age group highly represented (48.60%). Most participants
(88.60%) lived in urban areas and 51.43% had a non-liberal profession,the
majority (66.30%) lived as couples and 40.00% had a higher level of education.
Trip duration to the hospital was less than one hour for 84.60% of
participants. The high socioeconomic status was greatly represented in this
study (60%) and 10.9% of participants had a health insurance.
The High Normal BP group was most represented (24.60%) and
57.70% had a controlled BP. The most frequently encountered comorbidity was
heart failure (24.57%). Only 18.29% of participants had a handicap.
Calcium channel blockers were the most encountered monotherapy
(31.90%). The majority of participants took less than 3 different
antihypertensive. The mean treatment cost was 14543 #177; 8613FCFA and most
participants were in the 10000-20000FCFA monthly drug cost range. More than 90%
of participants were on a once daily posology 65.70% were on monotherapy.
Specialty medications were prescribed in most cases (88.60%) and 38.30%
experienced side effects due to medication.
Poor adherence was observed in 32.60% of study
participants.After multivariate analysis with logistic regression, 9 variables
were significantly associated with poor adherence: first cycle secondary
education, living singly, trip duration of one hour or more, middle
socioeconomic status, uncontrolled BP status, presence of handicap,
monotherapy, presence of side effects, and taking medications in the
evening.
Of the 74 patients with uncontrolled BP, 86.49% had poor
adherence. Patients with uncontrolled BP were associated with poor therapeutic
adherence.
VI.2 RECOMMENDATIONS
At the end of this study, we formulate the following
recommendations:
· To the Ministry of Public Health,
1- To reinforce information, education and communication in
the whole country on non-communicable diseases especially hypertension, so that
patients should know the importance of adhering to antihypertensive treatments
prescribed.
2- To accelerate the implementation of the universal insurance
coverage in Cameroon so that patients could easily purchase their
antihypertensive drug prescribed.
· To Health Personnel,
1. Reinforce sensitization of patients with hypertension on
the need to adhere to their treatments which is lifelong in order to avoid
comorbidities and complications.
2. Insist on the need to prescribe generic drugs which are
less expensive in order to increase access and improve treatment adherence.
3. To opt for antihypertensive drugswhich have less side
effects and which are taken once daily to facilitate adherence.
CHAPTER VII:
REFERENCES
1. World Health Organization. A global brief on Hypertension:
Silent killer, global public health crisis. 2013. 39 p. Available from:
http://ish-world.com/downloads/pdf/global_brief_hypertension.pdf. Consulted on:
18/09/2016.
2. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K,
Adair-Rohani H, et al. A comparative risk assessment of burden of disease and
injury attributable to 67 risk factors and risk factor clusters in 21 regions,
1990-2010: a systematic analysis for the Global Burden of Disease Study 2010.
Lancet. 2012;380(9859):2224-60.
3. Sweetman SC. Martindale: The Complete Drug Reference.
Thirty-sixth edition. Great Britain: Pharmaceutical Press; 2009. 3709 p.
4. World Health Organization. Global status report on
noncommunicable diseases. WHO; 2010.p. 1-176. Available from:
http://www.who.int/nmh/publications/ncd_report_full_en.pdf. Consulted on:
18/09/2016.
5. MM Finucane, GA Stevens, M Cowan, Goodarz D, JK Lin, CJ
Paciorek, et al.. National, regional, and global trends in systolic blood
pressure since 1980: systematic analysis of health examination surveys and
epidemiological studies with 786 country-years and 5.4 million participants.
Lancet. 2011; 377(9765): 557-67.
6. World Health Organization. World Health Statistics. 2015.
161 p. Available from:
http://apps.who.int/iris/bitstream/10665/170250/1/9789240694439_eng.pdf?ua=1.
Consulted on: 14/12/2016.
7. Ambaw AD, Alemie GA, Yohannes SM, Mengesha ZB. Adherence
to antihypertensive treatment and associated factors among patients on follow
up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health.
2012;12:282-8.
8. Kingue S, Ndong Ngoe C, Menanga AP, Jingi AM, Noubiap JJN,
Fesuh B, et al. Prevalence and Risk Factors of Hypertension in Urban Areas of
Cameroon: A Nationwide Population-Based Cross-Sectional Study. J Clin
Hypertens. 2015;17(10):819-24.
9. Kamadjeu R, Edwards R, Atanga J, Unwin N, Kiawi E, Mbanya
J-C. Prevalence, awareness and management of hypertension in Cameroon: findings
of the 2003 Cameroon Burden of Diabetes Baseline Survey. J Hum Hypertens.
2006;20(1):91-2.
10. Osterberg L, Blaschke T. Adherence to Medication. N Engl J
Med. 2005; 353(5):487-97.
11. Department of Economic and Social Affairs, Population
Division. World Population Prospects: The 2015 Revision. 2015. 59 p. Available
from: https://esa.un.org/unpd/
wpp/publications/files/key_findings_wpp_2015.pdf. Consulted on:
14/12/2016.
12. Chaves ES, Lucio IM, de Araújo TL, Damasceno MM.
Efficiency of health education programs for adults with high blood pressure.
Rev Bras Enferm. 2006; 59(4):543-7.
13. Saleem F, Hassali M, Shafie A, Awad A, S Bachir.
Association between Knowledge and Drug Adherence in Patients with Hypertension
in Quetta, Pakistan. Trop J Pharm Res. 2011; 10(2):125-32.
14. Ho PM, Magid DJ, Shetterly SM, Olson KL, Peterson PN,
Masoudi FA, et al. Importance of Therapy Intensification and Medication
Nonadherence for Blood Pressure Control in Patients With Coronary Disease. Arch
Intern Med. 2008;168(3):271-6.
15. Balkrishnan R. The Importance of Medication Adherence in
Improving Chronic-Disease Related Outcomes: What We Know and What We Need to
Further Know. Med Care. 2005; 43(6):517-20.
16. Mbouemboue OP, Tamanji MT, Gambara R, Lokgue Y, Ngoufack
JO. Determinant therapeutic nonadherence to antihypertensive treatment: a
hospital-based study outpatients in Northern Cameroon. Int J Med Sci Public
Health. 2016; 5(3):547-54.
17. Mbouemboue OP, Milamem NAA, Tamanji MT, Atanga MB.
Educational Need Hypertensive Patients in Buea Hospital Setting. Health Sci
Dis. 2016; (2):1-5.
18. Tufon EN, Forstabel FB, Christian NT. Adherence to
Antihypertensive Treatment Factors Associated with Adherence Amongst
Hypertensive Patients on Follow-up at Mankon Sub-Divisional Health Center,
Ntingkang, Bamenda, Cameroon. VRI Signaling. 2014; 2(1):27-31.
19. Essomba NE, Ba H, Koum DCK, Atemkeng A, Coppieters Y.
Facteurs de Non Observance au Traitement AntiHypertenseur chez les Adultes
à Douala. Health Sci Dis. 2017;18(3): 51-7.
20. Akoko BM, Fon PN, Ngu RC, Ngu KB. Knowledge of
Hypertension and Compliance with Therapy Among Hypertensive Patients in the
Bamenda Health District of Cameroon: A Cross-sectional Study. Cardiol Ther.
2017;6(1):53-67.
21. Rabbia F, Fulcheri C, Di Monaco S, Covella M, Perlo E,
Pappaccogli M, et al. Adherence to antihypertensive therapy and therapeutic
dosage of antihypertensive drugs. High Blood Press. Cardiovasc Prev.
2016;23(4):341-5.
22. Economic and Social Council. Progress towards the
Sustainable Development Goals. United Nations. 2016. p. 1-28. Report No.: 75.
Available from: https://daccess-ods.un.org/TMP/3127616.64390564.html. Consulted
on: 28/02/2017.
23. World Health Organization. Adherence to long-term therapies:
Evidence for action. 2003. 194 p. Available from:
http://apps.who.int/iris/bitstream/10665/42682/1/
9241545992.pdf. Consulted on: 01/12/2017.
24. M Molla, JH Madans, WK Wagener, EM Crimmins. Summary
measures of population health: Report of findings on methodologic and data
issues. 2003; p. 66. Available from:
https://www.cdc.gov/nchs/data/misc/pophealth.pdf. Consulted on: 01/07/2017.
25. World Health Organization. The global burden of disease.
WHO. 2004. p. 160. Available from:
http://www.who.int/healthinfo/global_burden_disease/
GBD_report_2004update_full.pdf. Consulted on: 18/09/2016.
26. Fezeu L, Kengne A, Balkau B, Awah PK, Mbanya J. Ten-year
change in blood pressure levels and prevalence of hypertension in urban and
rural Cameroon. J Epidemiol Community Health. 2010;64(4):360-5.
27. Echouffo-Tcheugui JB, Kengne AP. Chronic non-communicable
diseases in Cameroon burden, determinants and current policies. Global Health.
2011;7:44-53.
28. Dzudie A, Kengne AP, Muna WFT, Ba H, Menanga A, Kouam CK,
et al. Prevalence, awareness, treatment and control of hypertension in a
selfselected sub-Saharan African urban population: a cross-sectional study. BMJ
Open. 2012;2:e001217.
29. Varon J, Marik PE. Perioperative hypertension management.
Vasc Health Risk Manag. 2008; 4(3): 615-27.
30. Kintiraki E, Papakatsika S, Kotronis G, Goulis DG, Kotsis
V. Pregnancy-Induced hypertension. Hormones. 2015;14(2):211-23.
31. Cheung BMY, Li C. Diabetes and Hypertension: Is There a
Common Metabolic Pathway? Curr Atheroscler Rep. 2012;14(2):160-6.
32. JSH 2014. Chapter 13. Secondary hypertension.
Hypertension Research. 2014. 37: 349-61.
33. Carretero OA, Oparil S. Essential Hypertension: Part I:
Definition and Etiology. Circulation. 2000;101(3):329-35.
34. Ian Phillips M. Gene Therapy for Hypertension: The
Preclinical Data. Hypertension. 2001;38(3 Pt 2):543-8.
35. Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B,
Ferri C, et al. A Prospective Study of the Prevalence of Primary Aldosteronism
in 1,125 Hypertensive Patients. J Am Coll Cardiol. 2006;48(11):2293-300.
36. Omura M, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T.
Prospective Study on the Prevalence of Secondary Hypertension among
Hypertensive Patients Visiting a General Outpatient Clinic in Japan. Hypertens
Res. 2004;27(3):193-202.
37. American Heart Association. Understanding and Managing High
Blood Pressure. 2014. Available from:
http://dhhs.ne.gov/publichealth/WMHealth/Documents/
Understanding_Managing_HBP.pdf. Consulted on: 28/12/2016.
38. Beisl Noblat AC, Lopes MB, Lopes GB, Lopes AA.
Complications of Hypertension in Men and Women Seen in a Referral Outpatient
Care Unit. Arq. Bras. Cardiol.. 2004.83(4):314-9.
39. World Health Organization. Affordable Technology?: Blood
Pressure Measuring Devices for Low Resource Settings. Geneva. 2005. 26 p.
Available from: http://whqlibdoc.who.
int/publications/2005/9241592648.pdf. Consulted on:
22/12/2016.
40. Mancia G, de Backer G, Dominiczak A, Cifkova R, Fagard R,
Germano G, et al. 2007 Guidelines for the Management of Arterial Hypertension.
J Hypertens. 2007;25(6):1105-87.
41. Mancia G, Ferrari A, Gregorini L, Parati G, Pomidossi G,
Bertinieri G, et al. Blood Pressure and Heart Rate Variabilities in
Normotensive and Hypertensive Human Beings. Circ Res. 1983;53(1):96-104.
42. Modesti PA, Morabito M, Bertolozzi I, Massetti L, Panci
G, Lumachi C, et al. Weather-Related Changes in 24-Hour Blood Pressure Profile
Effects of Age and Implications for Hypertension Management. Hypertension.
2006;47(2):155-61.
43. O'Brien E, Waeber B, Parati G, Staessen J, Myers MG.
Blood pressure measuring devices: recommendations of the European Society of
Hypertension. BMJ. 2001; 322(7285): 531-6.
44. Clement DL, De Buyzere ML, De Bacquerb D, de Leeuw PW,
Duprez DA, Fagard RH, et al. Prognostic Value of Ambulatory Blood-Pressure
Recordings in Patients with Treated Hypertension. N Engl J Med.
2003;348(24):2407-15.
45. Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G,
Grassi G, et al. Prognostic Value of Ambulatory and Home Blood Pressures
Compared With Office Blood Pressure in the General Population: Follow-Up
Results From the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA)
Study. Circulation. 2005;111(14):1777-83.
46. Fagard R, Van Den Broeke C, De Cort P. Prognostic
significance of blood pressure measured in the office, at home and during
ambulatory monitoring in older patients in general practice. J Hum Hypertens.
2005;19(10):801-7.
47. Parati G, Pomidossi G, Casadei R, Mancia G. Lack of
alerting reactions to intermittent cuff inflations during noninvasive blood
pressure monitoring. Hypertension. 1985; 7(4):597-601.
48. Mancia G, Omboni S, Parati G, Ravogli A, Villani, A,
Zanchetti A. Lack of Placebo Effect on Ambulatory Blood Pressure. Am. J.
Hypertens. 1995;8(3):311-5.
49. Staessen JA, Thijs L, Fagard R, O'Brien E, Clement D, de
Leeuw PW, et al. Predicting Cardiovascular Risk Using Conventional vs
Ambulatory Blood Pressure in Older Patients With Systolic Hypertension. JAMA.
1999;282(6):539-46.
50. O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo
G, et al. European Society of Hypertension Position Paper on Ambulatory Blood
Pressure Monitoring. J Hypertens. 2013;31(9):1731-68.
51. Benetos A, Rudnichi A, Thomas F, Safar M, Guize L.
Influence of Heart Rate on Mortality in a French Population. Hypertension.
1999;33(1):44-52.
52. Alasdair Millar J. The Cockroft and Gault formula for
estimation of creatinine clearance: a friendly deconstruction. N Z Med J.
2012;125(1350):119-22.
53. Rydén L, Standl E, Bartnik M, Van den Berghe G,
Betteridge J, de Boer M-J, et al. Guidelines on diabetes, pre-diabetes, and
cardiovascular diseases: executive summary. Eur Heart J. 2007;28(1):88-136.
54. Ridker PM. High-Sensitivity C-Reactive Protein.
Circulation. 2001;103:1813-8.
55. Ridker PM, Buring JE, Cook NR, Rifai N. C-Reactive
Protein, the Metabolic Syndrome, and Risk of Incident Cardiovascular Events.
Circulation. 2003;107(3):391-7.
56. Andersson OK, Almgren T, Persson B, Samuelsson O, Hedner
T, Wilhelmsen L. Survival in treated hypertension: follow up study after two
decades. BMJ. 1998;317(7152):167-71.
57. Whitworth JA; World Health Organization, International
Society of Hypertension Writing Group. 2003 World Health Organization
(WHO)/International Society of Hypertension (ISH) statement on management of
hypertension. J Hypertens. 2003;21(11):1983-92.
58. Elmer PJ, Obarzanek E, Vollmer WM, et al. Effects of
comprehensive lifestylemodification on diet, weight, physical fitness, and
blood pressure control: 18-month results of a randomized trial. Ann Intern Med.
2006;144(7):485-95.
59. Whitworth JA; World Health Organization, International
Society of Hypertension Writing Group. 2003 World Health Organization
(WHO)/International Society of Hypertension (ISH) statement on management of
hypertension. J Hypertens. 2003;21(11):1983-92.
60. Williams B, Poulter N, Brown M, Davis M, McInnes G,
Potter J et al.. Guidelines for management of hypertension: report of the
fourth working party of the British Hypertension Society, 2004--BHS IV. J Hum
Hypertens. 2004;18(3):139-85.
61. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA,
Izzo JL Jr, et al.. The Seventh Report of the Joint National Committee on
Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA.
2003;289(19):2560-72.
62. Whelton PK, He J, Appel LJ, et al. Primary prevention of
hypertension: Clinical and public health advisory from the national high blood
pressure education program. JAMA. 2002;288(15):1882-8.
63. Chaudhry SI, Krumholz HM, Foody J. Systolic hypertension
in older persons. JAMA. 2004;292(9):1074-80.
64. Gueyffier F, Bulpitt C, Boissel J-P, Schron E, Ekbom T,
Fagard R, et al. Antihypertensive drugs in very old people: a subgroup
meta-analysis of randomized controlled trials. Lancet. 1999;353(9155):793-6.
65. Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L,
Dumitrascu D, et al. Treatment of Hypertension in Patients 80 Years of Age or
Older. N Engl J Med. 2008;358(18):1887-98.
66. Hansson L, Zanchetti A, Carruthers SG, Dahlöf B,
Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and
low-dose aspirin in patients with hypertension: principal results of the
Hypertension Optimal Treatment (HOT) randomised trial. Lancet.
1998;351(9118):1755-62.
67. Rosendorff C, Black HR, Cannon CP, Gersh BJ, Gore J, Izzo
JL, et al. Treatment of Hypertension in the Prevention and Management of
Ischemic Heart Disease. Circulation. 2007;115(21):2761.
68. Jackson R, Bellamy M. Antihypertensive drugs. BJA Educ.
2015;15(6):280-5.
69. Beta-Blockers in Thyrotoxicosis. The Lancet. 1980;315(8161):
184-6.
70. Hayes PE, Schulz SC. Beta-blockers in anxiety disorders. J
Affect Disord. 1987;13(2):119-30.
71. Brunton LL, Lazo JS, Parker KL. Goodman & Gilman's:
The pharmacological basis of therapeutics. Eleventh Edition. New York; 2006.
72. Nice Guideline 127. Hypertension in adults: diagnosis and
management. 2011. 25 p. Available from:
https://www.nice.org.uk/guidance/cg127/resources/hypertension-in-adults-diagnosis-and-management-pdf-35109454941637.
Consulted on: 13/11/2017.
73. van Vark LC, Bertrand M, Akkerhuis KM, Brugts JJ, Fox K,
Mourad J-J, et al. Angiotensin-converting enzyme inhibitors reduce mortality in
hypertension: a meta-analysis of randomized clinical trials of
renin-angiotensin-aldosterone system inhibitors involving 158 998 patients. Eur
Heart J. 2012;33(16):2088-97.
74. Pepper GA. Pharmacology of Antihypertensive Drugs. J
Obstet Gynecol Neonatal Nurs. 1999;28(6):649-59.
75. Neaton JD1, Grimm RH Jr, Prineas RJ, Stamler J, Grandits
GA, Elmer PJ, et al. Treatment of mild hypertension study: Final results. JAMA.
1993;270(6):713-24.
76. Materson BJ, Reda DJ, Cushman WC, Massie BM, Freis ED,
Kochar MS, et al. SingleDrug Therapy for Hypertension in Men: A Comparison of
Six Antihypertensive Agents with Placebo. N Engl J Med. 1993;328(13):914-21.
77. Bennet N. Hypertension in the elderly. The Lancet.
1994;344(8920):447-50.
78. Brewster LM, van Montfrans GA, Oehlers GP, Seedat YK.
Systematic review: antihypertensive drug therapy in patients of African and
South Asian ethnicity. Intern Emerg Med. 2016;11(3):355-74.
79. Khan N, McAlister FA. Re-examining the efficacy of
â-blockers for the treatment of hypertension: a meta-analysis. CMAJ Can
Med Assoc J. 2006;174(12):1737-42.
80. The ALLHAT Officers and Coordinators for the ALLHAT
Collaborative Research Group. Major cardiovascular events in hypertensive
patients randomized to doxazosin vs chlorthalidone: The antihypertensive and
lipid-lowering treatment to prevent heart attack trial (allhat). JAMA.
2000;283(15):1967-75.
81. National Institute for Health and Clinical Excellence.
Hypertension: The Clinical management of primary hypertension in adults. 2011.
34 p; 127. Available from:
http://www.ehy.ee/docs/pics/NICE%20hypertension%202011.pdf. Consulted on:
01/08/2017.
82. Turnbull F, Blood Pressure Lowering Treatment Trialists'
Collaboration. Effects of different blood-pressure-lowering regimens on major
cardiovascular events: results of prospectively-designed overviews of
randomised trials. Lancet. 2003;362(9395):1527-35.
83. Messerli FH, Williams B, Ritz E. Essential hypertension.
Lancet. 2007;370(9587):591-603.
84. Moser M, Setaro JF. Resistant or Difficult-to-Control
Hypertension. N Engl J Med. 2006;355(4):385-92.
85. van den Bosch WJHM, Mol W, van Gerwen W, Thien T.
Withdrawal of antihypertensive drugs in selected patients. The Lancet.
1994;343(8906):1157.
86. Aylett MJ, Creighton P, Jachuck S, Newrick D, Evans A.
Withdrawing antihypertensive drugs. Lancet. 1994;343(8911):1512.
87. Jung O, Gechter JL, Wunder C, Paulke A, Bartel C, Geiger
H, et al. Resistant hypertension? Assessment of adherence by toxicological
urine analysis. J Hypertens. 2013;31(4):766-74.
88. Burnier M, Wuerzner G, Struijker-Boudier H, Urquhart J.
Measuring, Analyzing, and Managing Drug Adherence in Resistant Hypertension.
Hypertension. 2013;62(2):218-25.
89. Brinker S, Pandey A, Ayers C, Price A, Raheja P, Arbique
D, et al. Therapeutic Drug Monitoring Facilitates Blood Pressure Control in
Resistant Hypertension. J Am Coll Cardiol. 2014;63(8):834-5.
90. Ceral J, Habrdova V, Vorisek V, Bima M, Pelouch R, Solar
M. Difficult-to-control arterial hypertension or uncooperative patients? The
assessment of serum antihypertensive drug levels to differentiate
non-responsiveness from non-adherence to recommended therapy. Hypertens Res.
2011;34(1):87-90.
91. Steiner JF, Earnest MA. THe language of medication-taking.
Ann Intern Med. 2000;132(11):926-30.
92. Naderi SH, Bestwick JP, Wald DS. Adherence to Drugs That
Prevent Cardiovascular Disease: Meta-analysis on 376,162 Patients. Am J Med.
2012;125(9):882-7.
93. Tomaszewski M, White C, Patel P, Masca N, Damani R,
Hepworth J, et al. High rates of non-adherence to antihypertensive treatment
revealed by high-performance liquid chromatography-tandem mass spectrometry (HP
LC-MS/MS) urine analysis. Heart. 2014;100(11):855-61.
94. Lam WY, Fresco P. Medication Adherence Measures: An
Overview. BioMed Res Int. 2015;2015:1-12.
95. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive
Validity of A Medication Adherence Measure in an Outpatient Setting. J Clin
Hypertens. 2008;10(5):348-54.
96. Farmer KC. Methods for measuring and monitoring medication
regimen adherence in clinical trials and clinical practice. Clin Ther.
1999;21(6):1074-90.
97. Belknap R, Weis S, Brookens A, Au-Yeung KY, Moon G,
DiCarlo L, et al. Feasibility of an Ingestible Sensor-Based System for
Monitoring Adherence to Tuberculosis Therapy. PLoS One. 2013;8(1):e53373.
98. Chung O, Vongpatanasin W, Bonaventura K, Lotan Y, Sohns
C, Haverkamp W, et al. Potential cost-effectiveness of therapeutic drug
monitoring in patients with resistant hypertension. J Hypertens.
2014;32(12):2411-21
99. Young K, Teeters J, Benesch C, Bisognano J, Illig K.
Cost-effectiveness of treating resistant hypertension with an implantable
carotid body stimulator. J Clin Hypertens. 2009;11(10):555-63.
100. Geisler BP, Egan BM, Cohen JT, Garner AM, Akehurst RL,
Esler MD, et al. Cost-Effectiveness and Clinical Effectiveness of
Catheter-Based Renal Denervation for Resistant Hypertension. J Am Coll Cardiol.
2012;60(14):1271-7.
101. Haynes R, McDonald HP, Garg AX. Helping patients follow
prescribed treatment: Clinical applications. JAMA. 2002;288(22):2880-3.
102. Lin YP, Huang YH, Yang YC, Wu JS, Chang CJ, Lu FH.
Adherence to Antihypertensive Medications among the Elderly: A Community-based
Survey in Tainan City, Southern Taiwan. Taiwan Geriatr Gerontol.
2007;2(3):176-89.
103. Hashmi SK, Afridi MB, Abbas K, Sajwani RA, Saleheen D,
Frossard PM, et al. Factors Associated with Adherence to Anti-Hypertensive
Treatment in Pakistan. PLoS ONE. 2007;2(3):1-8.
104. Hussain S, Boonshuyar C, Ekram A. Non-Adherence To
Antihypertensive Treatment in Essential Hypertensive Patients in Rajshahi,
Bangladesh. AKMMC J. 2011;2(1):9-14.
105. Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa
E, Immordino V, et al. Adherence to Antihypertensive Medications and
Cardiovascular Morbidity Among Newly Diagnosed Hypertensive Patients.
Circulation. 2009;120(16):1598-605.
106. Demoner MS, Ramos ER de P, Pereira ER. Factors associated
with adherence to antihypertensive treatment in a primary care unit. Acta Paul
Enferm. 2012;25(1):27-34.
107. Behnood-Rod A, Rabbanifar O, Pourzargar P, Rai A, Saadat
Z, Saadat H, et al. Adherence to Antihypertensive Medications in Iranian
Patients. Int J Hypertens. 2016;1-14.
108. Hedna K, Hakkarainen KM, Gyllensten H, Jönsson AK,
Sundell KA, Petzold M, et al. Adherence to Antihypertensive Therapy and
Elevated Blood Pressure: Should We Consider the Use of Multiple Medications?
PLoS ONE. 2015;10(9):1-14.
109. Lo SHS, Chau JPC, Woo J, Thompson DR, Choi KC. Adherence
to Antihypertensive Medication in Older Adults With Hypertension. J Cardiovasc
Nurs. 2016;31(4):296-303.
110. Okwuonu CG, Uwanurochi NV, Chimezie OJ, Ogah OS, Mbanaso
AU, Odigwe CO. Adherence to antihypertensive medication and its correlates
among individuals with hypertension in a semi-urban community of Southern
Nigeria. JMBR. 2015;14(1):5-17.
111. Boima V, Ademola AD, Odusola AO, Agyekum F, Nwafor CE,
Cole H, et al. Factors Associated with Medication Nonadherence among
Hypertensives in Ghana and Nigeria. Int J Hypertens. 2015;1 -8.
112. Charan J, Biswas T. How to Calculate Sample Size for
Different Study Designs in Medical Research? Indian J Psychol Med.
2013;35(2):121-6.
Prof, the Zotero program produces automatically the references.
Please are there some information lacking?
113. James PA, Oparil S, Carter BL, Cushman WC,
Dennison-Himmelfarb C, Handler J, et al.
2014 evidence-based guideline for the management of high blood
pressure inadults: report from the panel members appointed to the Eight Joint
National Committee. JAMA. 2014; 311(5):507-20.
114. Raj Guru MS, Shilpa S, Maheshwaran R. Revised socio-economic
status scale for urban
and rural India - Revision for 2015. Socioeconimica. 2015
4:167-74.
CHAPTER VIII: APPENDIX
APPENDIX 1
Section A
Section B
APPENDIX 2
INFORMED CONSENT FORM
Title of study: Adherence to
antihypertensive treatment and its associated factors in hypertensive patients
followed-up at the Yaounde General Hospital
Investigator:CHIABI Roland Muntoh
7th year pharmacy student
Faculty of Medicine and Biomedical Sciences - University of
Yaounde I
Tel: 693520478 E-mail: chiabiroland@gmail.com
Director: Pr MENANGA Alain Patrick
Co-director: Dr TEMBE Estella
épse FOKUNANG
Background:You are invited to take
part in a research study. Before you decide to participate in this study, it is
important you understand why the research is being done and what it will
involve. Please feel free to read through the following piece of information
and enquire from the investigator if there is anything ambiguous or if you need
more information.
Study aim: To assess the adherence
level and its associated factors to antihypertensive therapy among adult
hypertensive patients on follow-up in the Yaounde General Hospital.
Study procedure: Patients admitted
into this study shall be randomly and consecutively selected at the external
consultation cardiology service. After obtaining a written consent, we shall
proceed by measuring the resting blood pressure of each patient. Afterwards,
during an interview carried out in private, the investigator shall fill the
pretested questionnaires. Then, the questionnaires will eventually be collected
and safely stored to data analysis.
Benefits: By accepting to participate
in this study, you will directly help your healthcare providers to identify
your adherence issues. By so doing, adequate advice and support shall be
provided to you so that you adopt the right attitudes directed towards reducing
your high blood pressure.
Risks/Discomfort:There are virtually
no risks in participating in this study. A momentary discomfort could however
be felt while taking the blood pressure (i.e. when the cuff is inflated).
Participation: Participation in this
research study is voluntary. You have the right to withdraw at any time or
refuse to participate entirely without prejudice to the health care offered by
the hospital.
Ethics:Information you will provide
will be used for this study only and will not be shared for any other purposes
or projects.
Consent:I have read, understood, and
received a copy of the above consent form. I desire on my own free will to
participate in this study.
Yaounde, ..................................................
Signature of the investigator
Signature of the patient
FICHE DE CONSENTEMENT ECLAIRE
Titre de l'étude: Observance au
traitement antihypertenseur et ses facteurs associés chez les patients
hypertendus suivis à l'Hôpital Général de
Yaoundé
Enquêteur: CHIABI Roland Muntoh
Étudiant en 7e année de pharmacie
Faculté de Médecine et de Sciences
Biomédicales - Université de Yaoundé I
Tel: 693520478 E-mail: chiabiroland@gmail.com
Directeur: Pr MENANGA Alain Patrick
Codirecteur: Dr TEMBE Estella épse
FOKUNANG
Contexte: Vous êtes
invité à participer à un travail de recherche. Avant de
décider de participer à cette étude, il est important que
vous compreniez pourquoi la recherche a lieu d'être et ce qu'elle
impliquera. N'hésitez pas à lire l'information suivante et
à vous renseigner auprès de l'enquêteur s'il y a quelque
chose d'ambigu ou si vous avez besoin de plus d'information.
But de l'étude: Évaluer
le taux d'observance et ses facteurs associés au traitement
antihypertenseur chez les patients adultes hypertendus suivis à
l'Hôpital Général de Yaoundé.
Procédure: Les patients admis
dans cette étude seront sélectionnés de manière
aléatoire et consécutive dans les services externes de
consultation cardiologiques. Après avoir obtenu un consentement
écrit, nous procéderons en mesurant la pression artérielle
au repos de chaque patient. Ensuite, lors d'un échange en privé,
l'enquêteur remplira les questionnaires pré-testés. Les
questionnaires seront éventuellement collectés et rangés
en lieu sûr par l'investigateur pour l'analyse ultérieure des
données.
Avantages: En acceptant de participer
à cette étude, vous aiderez directement vos fournisseurs en soins
de santé à identifier vos problèmes d'observance. Ce
faisant, des conseils et un soutien adéquats vous seront fournis afin
que vous adoptiez les bonnes attitudes visant à réduire votre
tension artérielle élevée.
Risques/inconfort: Il n'y a
pratiquement aucun risque à participer à cette étude. Un
inconfort momentané peut toutefois être ressenti lors de la prise
de la pression sanguine (c'est-à-dire lorsque le brassard est
gonflé).
Participation: La participation
à ce travail de recherche est volontaire. Vous avez le droit de vous
retirer à tout moment ou de refuser de participer entièrement
sans préjudice des soins de santé offerts par l'hôpital.
Éthique: Les informations que vous
fournirez ne seront utilisées que pour cette étude et ne seront
pas partagées à d'autres fins ou projets.
Consentement: J'ai lu, compris et
reçu une copie du formulaire de consentement ci-dessus. Je désire
de mon plein gré participer à cette étude.
Yaoundé,
.......................................................
Signature de l'enquêteur
Signature du patient
APPENDIX 3: CASE REPORT FORM

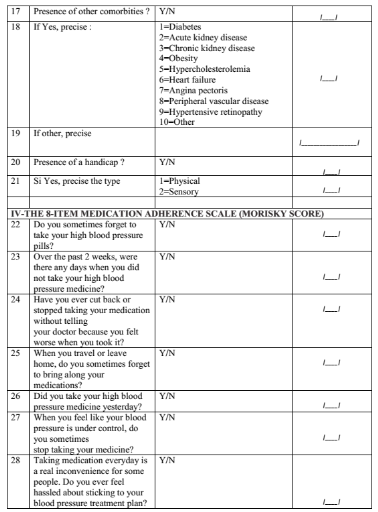
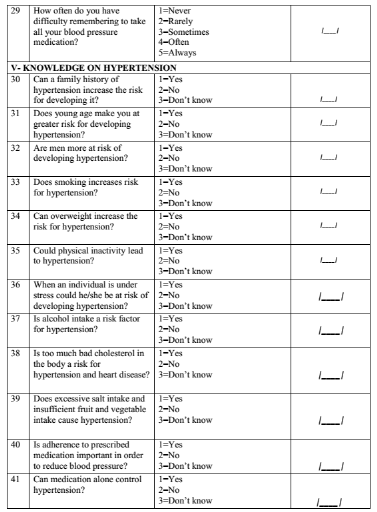

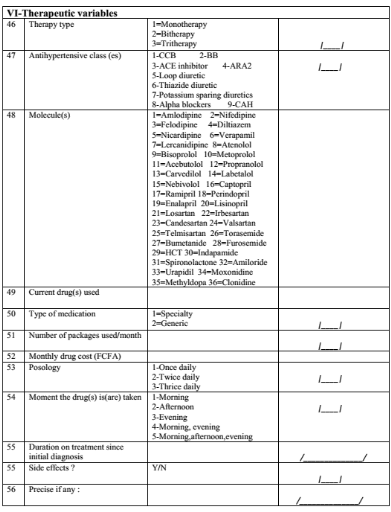 
| 


