V.5) HOSPITAL OUTCOME OF BACTERIAL MENINGITIS IN
CHILDREN
We recorded in our study 1 death representing 2.4 % of all the
children admitted for bacterial meningitis. This is very low compared to that
of Nguefack et al at YGOPH in 2014 with 17 deaths that is 53.1 % [3].
Koko in Gabon had much higher with 62 % [65].
However, our result had similarities with that of Wee LY et al in
Singapore who recorded 6 % of death cases [71]. Chandran had a
much lower percentage of 0.4% [6]. This low record of ours is
probable due to the early death of patients that were suspected of having
meningitis at entry, who died before any confirmatory examination notably
lumbar puncture could be performed probably because they presented with
contraindications.
We found that respiratory distress was the most common
complication of bacterial meningitis during hospitalization at 20.9 % at the
general pediatric unit at the YGOPH, followed by anemia with 16.3 %. We also
noted dehydration and status epilepticus as complications of meningitis both at
11.6 %. It is different from what Franco-Paredes and Nguefack had both with
seizure disorders and status epileticus as their main complication of bacterial
meningitis at 37 % and 54.7 % respectively[3][60].This result
can be explained by the fact that Streptococcus pneumoniae was the
predominant pathogen found , thus it is obvious for these patients to have
respiratory problems. The anemia can be justified by the fact that there must
have been an associated disease like malaria which is known to cause anemia
.Dehydration being present as a complication can be explained by the symptom of
fever, where fluid tends to be lost through sweat.
Hydrocephalus was the most common sequelae in the study at 9.3
% which is contradictory to that of Nguefack et al who had psychomotor
regression as the highest sequelae at 2.9 %3]. Sile had at the
Garoua provincial hospital 1 case of paraplegia [67].
Among the 4 patients that had hydrocephalus from our study, 2
had neurosurgery as treatment. This is probably due to poor financial
conditions that disabled the 2 others from benefiting from the treatment.Among
patients who had psychomotor regression (1)
51
and tetra paresis (2), 2 had physiotherapy done for their
rehabilitation, explained by probable poor financial conditions for the one
that could not afford for the service.
? LIMITATIONS OF THE STUDY
We encountered various difficulties of which some are
naturally found in every retrospective study that is: files with incomplete
information, files that were not exploitable, and many files were lost from the
archives because most of these files didn't return when they left this service
for another unit in the hospital. There was a problem of uniformity among the
health personnel too in taking clinical observations notably for the
diagnosis.
Also considering the fact that there were a limited number of
pathogens available, the antibiogramme sensitivity analysis could not be
done.
CONCLUSION
At the end of this study, the different specific objectives
have been attained. We can therefore come to the conclusion that:
> The incidence of bacterial meningitis in children at the
YGOPH is 0.3%.
> The most common etiologies responsible for bacterial
meningitis in YGOPH are Streptococcus pneumoniae at 63% and
Neisseria meningitidis at 25 % and presented more in children <12
months of age .
> Most children presented at the consultation with fever as
the predominant symptom at 95.3%, followed by convulsions at 60.5 %.On clinical
examination, neck stiffness was the most common sign at 20.9%, followed by
meningeal signs at 16.3%.
> The mortality was 2.4 %, and 97.6 % of patients left the
hospital alive .Among the 97.6 % patients that left the hospital alive, 61.5%
had neurological complications.
RECOMMENDATIONS
Our conclusions above enable us to do the following
recommendations;
? TO THE MINISTRY OF PUBLIC HEALTH
- Re-enforce vaccination campaigns in children all over the
country.
52
? YAOUNDE GYNECO-OBSTETRIC AND PEDIATRIC
HOSPITAL
- Re-enforce information towards infectious diseases especially
on meningitis.
- Re-enforce information, education and communication on
vaccinations of children.
53
REFERENCES
1. Oordt-Speets AM, Bolijn R, van Hoorn RC, Bhavsar
A, Kyaw MH.
Global etiology of bacterial meningitis: A systematic
review and meta-analysis. PloS One. 2018 Jun
11;13(6):e0198772.
2. Habtamu A, Sadikalmahdi H, Chelkeba L.
Childhood bacterial
meninigitis: Antimicrobial use pattern and
treatment outcomes: a prospective observational study.ClinPract. 2018;
15(SI):587-02.
3. Nguefack S, Chiabi A, Enoh J, Mah E, Kamga KK,
Tatah S,et al.
Etiologies and Outcome of Children with Purulent
Meningitis at the Yaounde Gyneco-Obstetric and Pediatric Hospital (Cameroon).
Open J Pediatr. 2014 Nov 3; 4(04):269-75.
4. Curtis S, Stobart K, Vandermeer B, Simel DL,
Klassen T. Clinical
features suggestive of meningitis in children:
a systematic review of prospective data. Pediatr. 2010 Nov 1; 126(5):952-60.
5. Zewdie AT. Prevalence,aetiology and
antimicrobial susceptibility of bacterial
neonatal meningitis at Tikur
Ambessa specialized Hospital, Addis Abbeba , Ethiopia
[Thesis].[Nairobi]:University of Nairobi; 2011.
6. Chandran A, Herbert H, Misurski D, Santosham M.
Long-term sequelae
of childhood bacterial meningitis: an
underappreciated problem.Pediatr Infect Dis J. 2011 Jan 1; 30(1):3-6.
7. Pelkonen T, Roine I, Monteiro L, Correia M,
Pitkäranta A, Bernardino
L et al. Risk factors for death and
severe neurological sequelae in childhood bacterial meningitis in sub-Saharan
Africa. Clin Infect Dis. 2009 Apr 15; 48(8):1107-10.
8. Touré FS, Kouame S, Tia H, Monemo P,
Cissé A, Diané B, et al.
Epidemiology of paediatric
meningitis in central Côte d'Ivoire after the implementation of
Haemophilus influenzae type b vaccination. Newmicrobiol. 2017 Jul 1;
40(3):170-4.
9. Robbins JB, Schneerson R, Gotschlich EC, Mohammed
I, Nasidi A,
Chippaux JP,et al. Meningococcal meningitis in
sub-Saharan Africa: the case for mass and routine vaccination with available
polysaccharide vaccines. Bull World Health Organ. 2003; 81:745-50.
10.
54
Johnson AW, Adedoyin OT, Abdul-Karim AA, Olanrewaju
AW. Childhood pyogenic meningitis: clinical and investigative
indicators of etiology and outcome. J Natl Med Assoc. 2007 Aug; 99(8):937.
11. Martin Health. United Nations Sustainable
Development; November 2018. Available from
https://www.un.org/sustainabledevelopment/health
[Assessed 06 Dec 2018]
12. WHO. Weekly epidemiological Record Who.
2011.Available from
https://www.who.int/wer/2011/wer8647
[Assessed 12 Dec 2018]
13. WHO. Epidemic meningitis control in
countries of the African meningitis belt Who.2018.Availablefrom
https://apps.who.int/iris/handle/10665/272297.
[Assessed Dec 2018]
14. Nadel S. Prospects for eradication of
meningococcal disease. Arch Dis child. 2012 Nov 1; 97(11):993-8.
15. WHO (CDS/CSR/EDC/99, 7.Laboratory methods
for the diagnosis of meningitis caused by Neisseria meningitidis ,
Streptococcus pneumoniae and Haemophilus influenza
who.1999.AvailablefromWhqlibdoc.who.int/hq/2011/WHO_IVB_11.09[Asse ssed 12 Dec
2018].
16. CDC.Pediatric. Bacterial meningitis
Surveillance-AfricanRegion(2002-2008).Available from
https://
wwwnc.cdc.gov>12-0375_article [Assessed Feb 2019]
17. Chacon-Cruz E, Alvelais-Palacios JA,
Lopatynsky-Reyes EZ, Rodriguez-Valencia JA, and Volker-Soberanes ML.
Meningococcal Disease in Children: Eleven Years of Active Surveillance in a
Mexican Hospital and the Need for Vaccination in the Tijuana Region. J Infec
Dis Treat. 2017;3:1.
18. Peltola H. Worldwide Haemophilus
influenzae type b disease at the beginning of the 21st century: global analysis
of the disease burden 25 years after the use of the polysaccharide vaccine and
a decade after the advent of conjugates. Clin microbiol Rev. 2000 Apr
1;13(2):302-17.
19. Gurley ES, Hossain MJ, Montgomery SP, Petersen
LR, Sejvar JJ, Mayer LW,et al. Etiologies of bacterial meningitis in
Bangladesh: results from a hospital-based study. Am J Trop Med.Hyg. 2009 Sep 1;
81(3):475-83.
20.
55
Immunopedia .Org. Streptococcal pneumoniae
meningitis 2011 -2019.
Availablefrom
https://www.immunopaedia.org.za/immunology/archive/immu
ne-evasion/blood-brain-barrier/iga-complement/streptococcal-pneumoniae-meningitis[Assessed
02 Feb 2019].
21. Mellroth P , Daniels R, Eberhardt A, Ronnlund D ,
Blom H, Widengren J et al. Lyt A, major autolysin of Streptococcus
pneumoniae , requires access to nascent peptidoglycan.J Biol Chem .2012 Mar
30;287(14):11018-29.
22. Tacon CL, Flower O. Diagnosis and
management of bacterial meningitis in
the paediatric population: a review.
Emerg Med Int. 2012;2012 :320-09.
23. Chávez-Bueno S, McCracken GH.
Bacterial meningitis in children. Pediatr
Clin. 2005 Jun 1;
52(3):795-10.
24. Jauneikaite E, Mary Carnon Jefferies J, William
VereChurton N, Tzer Pin Lin R, Lloyd Hibberd M, Charles Clarke S.
Genetic diversity of Streptococcus pneumoniae causing meningitis and
sepsis in Singapore during the first year of PCV7 implementation. Emerg
Microbes Infect. 2014 Jan 1;3(1):1-7.
25. Aviq. Infection invasive à
Haemophilus influenza type b. Juillet 2016.
Available from
https://www.wiv-isp.be>H_influenzae
[assessed May 2019]
26. Rosadini C. Roles of secreted virulence
factors in pathogenecity of
Haemophilus influenzae: A Dissertation, United
States of America [Thesis].[Massachusetts]:University of Massachusetts medical
school;2011.
27. Naik DG, Seyoum M. Haemophilus
influenzae type b meningitis in children,
Eritrea. Emerg Infect Dis. 2004
Jan;10(1):155-6.
28. Greenberg-Kushnir N, Haskin O, Yarden-Bilavsky H,
Amir J, Bilavsky E. Haemophilusinfluenzae type b meningitis in the
short period after vaccination: a reminder of the phenomenon of apparent
vaccine failure. Case Rep Infect Dis. 2012;2012 : 950-07.
29. Manchanda V, Gupta S, Bhalla P.
Meningococcal disease: history,
epidemiology, pathogenesis,
clinical manifestations, diagnosis, antimicrobial susceptibility and
prevention. Indian J Med Microbiol. 2006 Jan 1;24(1):7-19.
30. Hart CA, Thomson AP. Meningococcal
disease and its management in children. BMJ. 2006 Sep 28; 333(7570):685-90.
31.
56
Thigpen MC, Whitney CG, Messonnier NE, Zell ER,
Lynfield R, HadlerJL,et al. Bacterial meningitis in the United States,
1998-2007.Engl J Med. 2011 May 26; 364(21):2016-25.
32. WHO. Meningococcal vaccines, November2011,
Weekly Epidemiological
Record[Internet]Who.2011.Available from
https://www.who.int/wer/2011/wer8647
[Assessed 03 Feb 2019].
33. Rouphael N.G, Stephens D.S. Neisseria
meningitidis: Biology, microbiology
and epidemiology. Methods Mol Biol.2012;
799: 1-20.
34. Al-Ani MM. Risk Factors of Meningitis in
Children Under Five Years in Al-
Ramadi Maternity and Children Hospital.
Al-Anbar Med J. 2009;7(1):76-84.
35. Al Jarousha AM, Al Afifi A. Epidemiology
and risk factors associated with
developing bacterial meningitis among
children in Gaza Strip. Iran J PublHealth. 2014 Sep;43(9):1176-83.
36. Shapiro ED, Aaron NH, Wald ER, Chiponis D.
Risk factors for development of bacterial meningitis among children
with occult bacteremia. J Pediatr. 1986 Jul 1;109(1):15-9.
37. Borrow R, Caugant DA, Ceyhan M, Christensen H,
Dinleyici EC, Findlow J, et al. Meningococcal disease in the Middle
East and Africa: Findings and updates from the Global Meningococcal Initiative.
J Infect. 2017 Jul 1;75(1):1-1.
38. Hoffman O, Weber JR. Pathophysiology and
treatment of bacterial
meningitis. Ther Adv Neurol Discord. 2009
Nov;2(6):401-12.
39. Cohen ML. Changing patterns of infectious disease.
Nature.2000 Aug;406(6797):762-7.
40. Leib SL, Täuber MG. Pathogenesis of
bacterial meningitis. Infect Dis Clin
North Am. 1999 Sep 1; 13(3):527-48.
41. Baines P, Reilly P, Gill. Paediatric
meningitis: Clinical features and
diagnosis.ClinPharm .2009 Aug; 307-10.
42. Schulga P, Grattan R, Napier C, Babiker MO.
How to use... lumbar puncture in children. Arch Dis Child EducPract.
2015 Oct 1;100(5):264-71.
43. Hasbun R. Update and advances in
community acquired bacterial
meningitis.Curr Opin Infect Dis. 2019 Jun 1;
32(3):233-8.
44.
57
Gorn M, Kunkov S, Crain EF. Prospective
investigation of a novel
ultrasound-assisted lumbar puncture technique on
infants in the pediatric emergency department. Acad Emerg Med. 2017
Jan;24(1):6-12.
45. Saberi A., Roudbary S.A., Ghayeghran A., Kazemi
S.,Hosseininezhad
M.Diagnosis of meningitis caused by pathogenic
microorganism using magnetic resonance imaging ; A systematic review.Basic clin
Neurosci.2018 Apr ;9(2):736-86
46. Velissaris D, Pintea M, Pantzaris N, Spatha E,
Karamouzos V,
PierrakosC,et al. The role of procalcitonin in the
diagnosis of meningitis: a literature review. J Clin Med. 2018 Jun;7(6):148.
47. Swann O, Everett DB, Furyk JS, Harrison EM,
Msukwa MT,Heyderman RS,et al. Bacterial meningitis in Malawian
infants< 2 months of age: etiology and susceptibility to World Health
Organization first-line antibiotics. Pediatr Infect Dis J. 2014 Jun;
33(6):560-65.
48. WHO. Vaccination Who.2018.Available from
https://www.Who.Int/ immunization/p[Assessed on Aug 2019]
49. Makwana N., Riordan F. Bacterial
meningitis: the impact of vaccination
.CNS Drugs.2007.
50. Davis S., Feikin D., Johnson H.The
effect of Hib and pneumococcal
conjugates vaccines on childhood meningitis
mortality: A systematic review. BMC Public Health. 2013.
51. CDC. Pneumococcal vaccins. Available
from
https://www.cdc .gov>vpd
>
pneumo.[Assessed Aug 2019]
52. WHO. Pneumococcal vaccins
Who.2018.Available from
https://www.Who.Int >vaccines
pneumo.[Assessed Aug 2019]
53. WHO.Meningococcal vaccines Who. 2018.
Available from
https://www.Who.Int > Ith >
vaccines >meningitis.[Assessed Aug 2019]
54. WHO.Haemophilus influenza vaccins
Who.2015. Available from https://
www.Who.Int >diseases >hib.[Assessed
Aug 2019]
55. Sáez-Llorens X, McCracken Jr GH.
Bacterial meningitis in children.
Lancet. 2003 Jun
21;361(9375):2139-48.
56.
58
Heydari B, Khalili H, Karimzadeh I, Emadi-Kochak H.
Clinical,
paraclinical, and antimicrobial resistance features of
community-acquired acute bacterial meningitis at a large infectious diseases
ward in Tehran, Iran.Iran J Pharm Res. 2016;15(1):347-54.
57. Control and prevention of meningococcal
Disease.Recommendations of the
Advisory committee on immunization.
1997 Feb.14; 46(RR-5): 1-10.
58. De Souza AL, Sztajnbok J, Seguro AC.
Cerebellar hemorrhage as an atypical complication of meningococcal
meningitis. Int J Infect Dis. 2008 Sep 1;12(5):558-9.
59. Frank-Briggs AI, Alikor EA. Long term
neurological complications of
bacterial meningitis in Nigerian children.
Niger J Paed. 2013;40(3):295-8.
60. Mazankova LN, Milovanova OA, Moiseenkova DA,
Soldatova IA, Mikhalinova EP. Neurological presentations of bacterial
meningitis in children: current possibilities of diagnosis and treatment.
ZhNevrolPsikhiatr Im S SKorsakova. 2016;116(6):4-9.
61. Almuneef M, Memish Z, Khan Y, Kagallwala A,
Alshaalan M. Childhood bacterial meningitis in Saudi Arabia. J Infect.
1998 Mar 1;36(2):157-60.
62. Franco-Paredes C, Lammoglia L, Hernández
I, Santos-Preciado JI.
Epidemiology and outcomes of bacterial
meningitis in Mexican children: 10-year experience (1993-2003). Int J
Infect Dis. 2008 Jul 1;12(4):380-6.
63. Le Saux N. Antimicrobial stewardship in
daily practice: Managing an
important resource. Canad J Infect Dis Med
Microbiol. 2014;25(5):241-5.
64. Polkowska A, Toropainen M, Ollgren J,
Lyytikäinen O, Nuorti JP. Bacterial meningitis in Finland,
1995-2014: a population-based observational study. BMJ Open. 2017 May
1;7(5):e015080.
65. Shinjoh M, Yamaguchi Y, Iwata S.
Pediatric bacterial meningitis in
Japan,
2013-2015-3-5 years after the wide use of
Haemophilusinfluenzae type b and Streptococcus pneumoniae conjugated vaccines.
J Infect Chem. 2017 Jul 1;23(7):427-38.
66. Campagne G, Schuchat A, Djibo S, Ousseini A,
Cisse L, Chippaux JP. Epidemiology of bacterial meningitis in Niamey,
Niger, 1981-96. Bull World Health Organ. 1999;77(6):499-08.
67.
59
Koko J, Batsielili S, Dufillot D, Kani F, Gahouma D,
Moussavou A. Les
méningites bactériennes de l'enfant
à Libreville, Gabon. Aspects épidémiologiques,
thérapeutiques et évolutifs. Med Mal Infect. 2000 Jan
1;30(1):50-6.
68. Mullan PC, Steenhoff AP, Draper H, Wedin T,
Bafana M, AnabwaniG,et al. Etiology of meningitis among patients
admitted to a tertiary referral hospital in Botswana. Pediatr Infect Dis J.
2011 Jul 1;30(7):620-2.
69. Mefo HS, Sile H, Mbonda E, Fezeu R, Fonkoua MC.
Les méningites purulentes de l'enfant au Nord Cameroun: aspects
cliniques, bactériologiques et thérapeutiques. MédAfr
Noire. 1999;46(1):15 -20.
70. Fonkoua MC, Cunin P, Sorlin P, Musi J, Martin PM.
Bacterial meningitis
in Yaounde (Cameroon) in 1999-2000. Bull Soc
PatholExot(1990). 2001 Nov;94(4):300-3.
71. Gervaix A, Taguebue J, Bescher BN, Corbeil J,
Raymond F, AlcobaG,et al. Bacterial meningitis and pneumococcal
serotype distribution in children in Cameroon. Pediatr Infect Dis J. 2012 Oct
1;31(10):1084-7.
72. Fayyaz J, Rehman A, Hamid A, Khursheed M, Zia N,
Feroze A. Age related clinical manifestation of acute bacterial
meningitis in children. J Pak Med Assoc. 2014;64(3):296.
73. Otero Flórez JA, Gómez Navas MD,
Cornejo Ochoa JW, Cabrera Hemer DN. Clinical and paraclinical
characteristics in children with acute bacterial meningitis at the Hospital
Universitario San Vicente Fundación, in Medellín, Colombia.
2011-2015: descriptive-retrospective study. ActaNeurol Colom. 2017
Jun;33(2):84-93.
74. Wee LY, Tanugroho RR, Thoon KC, Chong CY, Choong
CT, Krishnamoorthy S,et al. A 15-year retrospective analysis of
prognostic factors in childhood bacterial meningitis. Acta Paediatr. 2016
Jan;105(1):e22-9.
75. Njapndounke T. Determinants de la
completitude vaccinale chez les enfants
ages de 0 à 11 mois à
L'hopitalGyneco-Obstetric et pédiatrique de Yaoundé, Cameroun
[Thèse].[Yaoundé]: Université de Yde 1;2016.
60
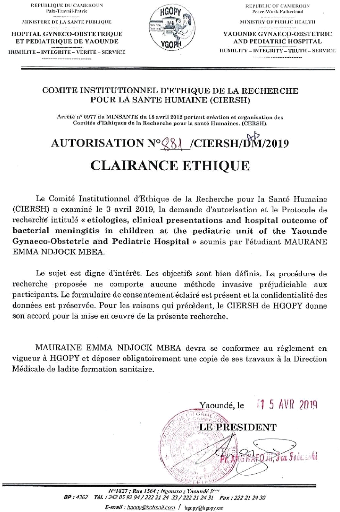
APPENDIX A : AUTORISATION OF THE YGOPH
APPENDIX B : QUESTIONNAIRE
A. IDENTIFICATION OF THE CHILD
Questionnaire N° File N°
Date of admission Weight
Date of birth Age
Sex M F
School level: pre-school primary secondary High school
Origin
Type of admission:CME/FCB Referred
Reason for admission
B. PAST HISTORY OF THE CHILD
1) Immunization calendar up to date yes No
i) If No, which vaccines lacks?
2) P24 statusyes No
i)If yes on treatment
3) Underlying disease yes No
i) If yes what disease
ii) Undergoing treatment for the
disease
4) Any contact with someone with meningitis before admission? Yes
No
C. INFORMATION ON THE PARENT / GUARDIAN
i)MOTHER
Age (years):<20 (20-34) >34
Profession: Liberal Non-liberal Student or pupil Not employed
Level of education: primary secondary higher education
illiterate
Matrimonial status: married single
Past medical history Region of
origin ..
ii)FATHER

Age (years):<20 (20-34) >34
Profession: Liberal Non-liberal Student or pupil Not employed
Level of education: primary secondary higher education
illiterate
Matrimonial status: married single
Past medical history Region of
origin ..
D. MANIFESTATION OF THE DISEASE ON THE CHILD

Convulsion yes No
Fever yes No
Kerning sign yes No
Brudzinski'ssign yes No
Nuchal rigidity yes No
Lethargy yes No
Bulging fontanelle yes No
Feeding problems yes No
Behavioural changes yes No
Respiratory manifestations yes No
i) If Yes which one
Digestive manifestations yes No
Others
E. LABORATORY FINDINGS ON CSF
1) Macroscopic examination of the
CSF/Appearance ..
2) CSF Biochemistry characteristics
Proteins g/dl
Glucose mmol/L
3) Cytology aspect of the CSF
WBC count cells/ml
RBC count cells/ml
4) Gram stain, bacteria isolated yes No
i) If yes what findings
5) Any CSF culture done yes No
If yes which growth was obtained
6)Soluble Antigens yes No
i)If Yes
F. OUTCOME DURING ADMISSION
Any complications yes No
i) If any, which one(s)
ii) Treatment received for the
complications
ii) Mortality yes No
Comorbidities: yes No .If yes which one(s)
G. EVOLUTION
cured Died Discharged against medical advice
H. TREATMENT RECEIVED i) Antibiotherapy
cephalosporins .Others
ii)Adjuvant therapy
Steroids anticonvulsant antipyretics
Iii) Fluid
I. PREVENTIVE MEARSURE
Preventive measures proposed? Yes No
i) If yes, which one?
Education on vaccination chemoprophylaxis of child at risk
| 


