In order to lay the theoretical and scientific foundations
for our work, it is essential to examine the research and solutions already
developed in similar fields. This chapter takes this approach by proposing an
in-depth analysis of what already exists, with the aim of placing our project
in its academic, medical and technological context. We begin by presenting the
key concepts relating to cardiovascular disease, with particular emphasis on
coronary artery disease, and the issues involved in training cardiology
students. We will then explore the contribution of immersive technologies, in
particular virtual reality, to medical learning. Particular attention will be
paid to existing applications of VR in cardiology, in order to identify
advances, shortcomings and future prospects. This review will identify the
foundations on which our approach is based, while justifying the relevance of
the proposed solution to improving specialized medical training.
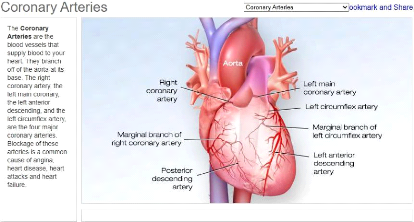
1.1 Coronary artery diseases
1.1.1 Overview
Cardiovascular diseases (CVDs) are a group of troubles
affecting the heart and blood vessels. They include conditions such as coronary
heart disease, cerebrovascular disease, rheumatic heart disease, and others
[10].
Among these, coronary artery disease (CAD) is one of the most
common and serious forms, and remains a major cause of morbidity and mortality
worldwide. Coronary artery disease occurs when the coronary arteries, which
supply oxygen-rich blood to the heart muscle, become narrowed or blocked. This
is typically the result of atherosclerosis, a process characterized by the
accumulation of fatty deposits (plaques) on the inner walls of the arteries.
Over time, these plaques harden and restrict blood flow to
the heart. If a plaque ruptures, it can cause a blood clot, leading to a heart
attack [9].
[9] The development of CAD is influenced by modifiable
lifestyle factors such as smoking, exces-
Chapter 1. State of Art 1.1. Coronary artery diseases
Figure 1.1: Coronary arteries
5
sive alcohol intake, poor diet, physical inactivity, and
chronic stress, as well as medical conditions including type 2 diabetes,
hypertension, and chronic kidney disease. Genetics and aging also contribute,
highlighting the importance of prevention and early detection.
Symptoms of CAD often appear gradually and can be subtle.
Typical signs include angina (chest pressure or pain), shortness of breath,
fatigue, dizziness, cold sweats, or nausea. Symptom presentation can vary by
sex, with men often exhibiting classic chest pain, while women may experience
atypical signs such as back or jaw discomfort, sleep disturbances, or anxiety.
This variability underscores the need for advanced training tools capable of
simulating diverse clinical scenarios to improve diagnosis and treatment
skills.
1.1.2 Coronary artery disease's treatments
Treatment of coronary artery disease (CAD) aims to relieve
symptoms, slow or reverse disease progression, and reduce the risk of heart
attacks and death. The therapeutic approach often depends on the severity of
the blockage, the presence of symptoms, and the overall health status of the
patient.
· Lifestyle and medical management:
In early or moderate stages, CAD may be managed through
non-invasive methods, including:
- Lifestyle modifications: Patients are
advised to stop smoking, reduce alcohol intake, adopt a healthy diet (e.g., low
in saturated fats and sodium), exercise regularly, and try to manage stress.
- Pharmacological treatments: they include
statins to lower cholesterol, beta-blockers to reduce heart rate and blood
pressure, antiplatelet agents such as aspirin to prevent clot formation, ACE
inhibitors and calcium channel blockers for blood pressure control, among
others.
These treatments are usually the first line of defense and may
significantly improve quality of life and prognosis.
· Chapter 1. State of Art 1.1. Coronary artery
diseases
6
Interventional procedures
When medical treatment is insufficient or significant
arterial blockage is present, more invasive procedures may be necessary. The
choice of procedure depends on the individual case and its severity, aiming to
achieve the best possible patient outcome.The most common procedures
include:
- Percutaneous Coronary Intervention
(PCI)
Also known as angioplasty, Percutaneous
Coronary Intervention (PCI) is a minimally invasive procedure to restore blood
flow in arteries narrowed or blocked by atherosclerotic plaque. During the
procedure, a flexible catheter is carefully inserted through the groin or wrist
and guided to the heart. Once at the blockage, a small balloon is inflated to
widen the artery, and in most cases, a stent is then placed to keep the artery
open.
PCI is a cornerstone of modern cardiology, indicated in acute
cases like STEMI as an emergency reperfusion strategy, in high-risk NSTEMI or
unstable angina patients, and in chronic CAD when symptoms persist despite
optimal medical therapy or when significant multi-vessel or left main disease
is present.
Instruments and medical equipment used
The setup for PCI requires specialized lab infrastructure and a
comprehensive arsenal of
instruments to safely treat coronary artery disease. We can
mention [18]:
* Operating table;
* Catheters (guide catheters, balloon catheters and aspiration
catheters);
* Stents ;
* Contrast dye;
* Guidewires ;
* Fluoroscopy and imaging equipment called angiography suite ( a
C-arm X-ray ma-
chine or biplane imaging system, digital monitors for live
image display, radiation
protection systems and integrated control consoles for the
interventional team);
* Pressure transducers and hemodynamic monitors;
* Sheaths and introducers;
* Cardiac defibrillator and emergency resuscitation
equipment;
* Patient monitoring system (ECG, pulse oximeter, etc.) ;
Risks, complications, and how they are
managed
Although Percutaneous Coronary Intervention (PCI) is generally
safe and routine, it carries some risks typical of invasive procedures. Most
complications are rare, but awareness is crucial for clinical practice and
understanding patient outcomes. Common risks include: * Bleeding or
hematoma at the catheter insertion site, especially with femoral
access. That's why careful post-procedure monitoring is essential. Manual
compression or vascular closure devices are often used to prevent
complications.
* Allergic reactions to the contrast dye can
occur, particularly in patients with a history of allergies or kidney issues.
In such cases, premedication or low-osmolar contrast agents are usually
recommended.
Chapter 1. State of Art 1.1. Coronary artery diseases
7
* Vascular injuries, like arterial dissection
or perforation, are rare but serious. These may require immediate endovascular
repair or, in extreme cases, emergency surgery.
* Arrhythmias (irregular heartbeats) might
happen during the procedure when instruments pass through the coronary
arteries. Most of the time, they're brief and managed with medications or
temporary pacing if needed.
* There's also a chance of restenosis
(artery narrowing again) or heart attack, but the use of drug-eluting
stents and dual antiplatelet therapy (DAPT) has significantly reduced this risk
over time.
In real-life practice, managing complications depends on a
skilled medical team, close monitoring, and good planning before the procedure.
Overall, the benefits of PCI clearly outweigh the risks ,especially for
patients with severe angina or acute heart attacks.
- Coronary Artery Bypass Grafting (CABG)
Coronary Artery Bypass Grafting (CABG) is a major heart
surgery with the same aim as the PCI defined above: to treat coronary
obstructions.
However,its technique is special: to «bypass» the
blocked arteries. Surgeons take a healthy blood vessel,often from the patient's
leg (saphenous vein) or chest (mammary artery) and graft it onto the heart to
reroute blood flow around the blockage. It's like building a new road when the
highway is closed.
CABG becomes necessary when medications and lifestyle changes
aren't enough or angioplasty (with stents) isn't a good option or the blockages
are too many or too complex.
Patients who benefit most from CABG usually have multiple
blocked arteries or diabetes or reduced heart function (especially in the left
ventricle).
Instruments and medical equipment used
Coronary Artery Bypass Grafting (CABG) relies on specialized
instruments and machines that support every stage of the complex surgery, from
opening the chest to maintaining circulation and performing precise vessel
grafting. [20]
* Operation table, pressure transducers, hemodynamic monitors
and patient monitoring system (ECG, Pulse oximeter, etc.) as for PCI ;
* Heart-Lung machine (Cardiopulmonary Bypass Machine);
* Dissection instruments ( scissors, forceps, scalpels, sternal
saws, and dissectors);
* Cannulae (arterial and venous tubes);
* Vascular grafts;
* Surgical retractors;
* Surgical sutures and needle holders; * Electrocautery
devices;
* Perfusion systems;
* Suction devices;
* Aortic punch and clamp [21] ;
Chapter 1. State of Art 1.2. Cardiology training issues
8
Risks, complications, and how they are
managed [23]
Even though Coronary Artery Bypass Grafting is a common and
life-saving surgery, it's important to understand that it comes with its share
of risks and possible complications. Some of the main risks include infections
at the incision site, bleeding during or after surgery, and issues related to
anesthesia. There's also a risk of irregular heart rhythms, like atrial
fibrillation, which can happen after surgery and may require medication or
further treatment.
More serious but less common complications can involve
stroke, heart attack, kidney problems, or lung issues. The surgical team is
always prepared to monitor for these and manage them quickly. For example,
antibiotics are given to prevent infection, and blood thinners may be used to
reduce the risk of clots.
Doctors also closely watch the patient's vital signs and use
advanced monitoring to catch any problems early. The recovery period includes
careful follow-up to ensure the heart is healing well and the new grafts remain
open.
1.2 Cardiology training issues
1.2.1 Current methods of training cardiology students
with contextual focus on Benin
In Benin, most of the cardiology education for future
specialists begins at the large Faculty of Health Sciences ( FSS ) of the
University of Abomey Calavi (UAC).
The FSS offers the degree called "Diplôme d'Études
Spécialisées des Maladies du Coeur et des Vaisseaux"[44, 45],
which includes theoretical lectures, classroom case studies, and occasional
practical exposure in affiliated hospitals such as Cotonou's National
University Hospital Hubert Koutoukou Maga.
Clinical rotations are mostly done at teaching hospitals like
the cardiology unit of the University Hospital in Cotonou, where students
observe procedures like ECGs, diagnostic angiographies, or rounds in
consultation and emergency services.[24] Unfortunately, due to limited
infrastructure and a high patient to student ratio, hands-on opportunities are
rare. The learning remains largely observation-based, with medical interns and
residents performing most interventions. According to some of those
students,theoretical knowledge is reinforced through seminars, lectures, and
case discussions led by senior cardiologists. However, advanced simulation
tools or structured procedural training labs are largely absent. The reliance
on traditional pedagogy reflects broader resource constraints in the health
sector and highlights a gap between classroom learning and actual clinical
competence. And in the end, their first real experience still happens directly
on a human patient.
1.2.2 Limitations of the theoretical approach
alone
In medical training,especially in cardiology,theoretical
knowledge is indispensable. However, it has a critical flaw: it prepares
students to know, but not necessarily to do.
In Benin, as in many countries with limited access to simulation
technologies,the only option left is to «learn on the
job», with all the risks that entails. Then, students often move
directly from theory to real-life practice... on real patients.
This situation raises both educational and ethical
concerns.
Chapter 1. State of Art 1.2. Cardiology training issues
9
A student might learn, in theory, how to manage a myocardial
infarction or perform an angioplasty, but their first real attempt often takes
place on an actual patient. There is no buffer, no rehearsal stage. Classrooms
teach equations and diagrams but not stress, uncertainty, or the weight of
holding a catheter when someone's life is at stake.
The result?
· Students feel unprepared and insecure, especially in
high-stakes procedures like those found in interventional cardiology.
· Patients, often unaware, become the first practice
ground, exposing them to potential risks.
· Instructors struggle to bridge the gap between
abstract knowledge and real-time performance under pressure for their
students.
This theory-practice gap is not a new problem. It has been
widely documented in international research. A study published in BMC Medical
Education (2020) highlights that students without early exposure to
simulation-based practice experience higher anxiety levels and reduced
performance in clinical situations. [25, 26]
1.2.3 Complication and error rates in initial coronary
surgery experiences
Several studies have documented measurable differences in
operative performance and complication rates during a surgeon's first
procedures, particularly in coronary artery bypass grafting (CABG).A
retrospective study conducted between 2008 and 2014 analyzed 1,668 CABG cases
performed by 21 surgical residents, each of whom had performed between 32 and
101 procedures under supervision. In their first 30 cases, residents
demonstrated a significantly longer operative time, an average of 29.7
minutes longer than experienced surgeons. This delay was
attributed primarily to longer incision-to-bypass
times (+13 minutes) and extended closure durations.
Importantly, these extended operative times did not correspond with higher
30-day mortality rates or major postoperative complications. [27].
In a separate analysis using data from the Society of
Thoracic Surgeons (STS) Adult Cardiac Surgery Database, 1,195 robotic-assisted
CABG procedures were evaluated across 114 surgeons with no prior experience in
robotic techniques. The first 10 cases for each surgeon revealed:
· A conversion rate drop from 7.7% to 2.5%,
· A major morbidity or mortality rate decline from 21.7% to
12.9%,
· A procedural success increase from 72.9% to 85.3% [28]
These findings confirm that the initial learning curve in
coronary surgery is associated with quantifiable performance differences,
particularly during the earliest procedures, despite adequate supervision and
safety measures.
1.2.4 Existing digital solutions (Excluding immersive
technologies)
Various non-immersive digital tools, including mobile apps,
web platforms, and simulation software, are used to train healthcare
professionals in cardiology, enhancing knowledge and clinical decision-making
skills.
· Chapter 1. State of Art 1.2. Cardiology training
issues
10
Touch Surgery (by Medtronic):
Touch Surgery is a mobile surgical simulation app used
globally to teach step-by-step procedures in various specialties, including
cardiovascular surgery. It offers interactive, gamified modules that guide
learners through virtual procedures using touchscreen gestures and 3D
animations.

Figure 1.2: Touch Surgery (by Medtronic)
· WebSurg :
WebSurg is a free online surgical training platform developed
by the IRCAD (Research Institute against Digestive Cancer). It provides a
comprehensive library of educational resources, including high-definition
surgical videos, expert commentaries, clinical case discussions, and
theoretical modules covering over 100 surgical procedures and specialties.It
supports multiple languages and is accessible worldwide, making it a valuable
tool, especially for professionals in regions with limited access to in-person
surgical training.
Figure 1.3: WebSurg home interface
· Surgery Squad:
Surgery Squad is an interactive web-based platform that
allows users to virtually perform various surgical procedures, such as coronary
bypass, appendectomies, and knee replacements, through guided, step-by-step
simulations. Designed primarily for educational outreach and
Chapter 1. State of Art 1.3. Immersive technologies in the
medical field
11
public engagement, it simplifies complex surgical processes and
makes them accessible to non-experts.
Figure 1.4: Surgery Squad home interface
1.3 Immersive technologies in the medical
field
Immersive technologies refer to digital systems designed to
simulate reality or extend it, allowing users to experience environments that
feel engaging, realistic, or entirely fabricated. These technologies create a
sense of «being there», often through multisensory input,visual,
auditory, and sometimes tactile making users feel mentally and physically
involved in the experience. Their core objective is to blur the line between
the physical and the digital world.[2] Several forms of immersive technologies
exist, each with specific characteristics and applications:
· Virtual Reality (VR): Fully immersive environments
where users are completely cut off from the physical world.
· Augmented Reality (AR): Overlays digital content onto
the real-world environment.
· Mixed Reality (MR): Combines real and virtual
environments with real-time interaction between physical and digital
objects.
Each of these technologies has made significant advances in
education, design, health, and entertainment. However, not all are equally
mature or widely implemented.
1.3.1 Virtual Reality as a key immersive technology in
medical training
While AR and MR are promising, Virtual Reality stands out
today as the most established and widely adopted immersive tool in medical
training. Its ability to simulate real-world procedures in a safe and
controlled environment without risk to patients has made it a go-to modality
for teaching anatomy, surgery, and complex decision-making. Its effectiveness
relies on three core pillars: presence (feeling «there» in the
virtual world), immersion (full sensory engagement), and interaction
(manipulating
Chapter 1. State of Art 1.3. Immersive technologies in the
medical field
12
virtual objects with immediate feedback), which together
transform passive learners into active participants, enhancing procedural
memory and reflex development.[30]
In addition, recent hardware improvements and decreasing
costs have made virtual reality more accessible to universities, hospitals, and
simulation centers around the world.
1.3.1.1 Types of Virtual Reality experiences in medical
education
All VR systems are not created equal. In medical education,
they are typically categorized into three main types, depending on their level
of immersion and technological complexity:
· Non-Immersive VR which is desktop-based, and allows
users to interact with 3D environments via a screen, keyboard, and mouse
without full sensory immersion. Despite its limitations, it enables students to
explore anatomy and simulate basic procedures.
· Semi-Immersive VR which uses large screens,
projectors, or CAVE systems to provide partial immersion. It enhances spatial
perception compared to non-immersive VR while still allowing real-world
interaction. These setups are ideal for group training or large-scale
visualizations.
· Fully Immersive VR which places users entirely inside
a virtual environment using head-mounted displays (HMDs), motion tracking, and
sometimes haptic feedback. Users' movements are mirrored in the simulation,
allowing precise surgical gestures and emergency responses.
1.3.1.2 Tools and equipment in VR training
To ensure effective medical training through VR, a
combination of specialized hardware and software is essential. These tools work
together to replicate real-life medical scenarios as closely as possible:
· Head-Mounted Displays (HMDs)
These wearable devices display the virtual environment and
track the user's head movements. Common models include Meta Quest 2 / Quest 3 ,
HTC Vive Pro and Pico Neo 3 / 4 .
· Motion controllers and hand tracking
Controllers enable interaction with virtual tools, such as
scalpels or syringes. More advanced systems support hand tracking, allowing the
user's hands to be visualized and used directly in the simulation. They are
useful in suturing, palpation, or tool manipulation.
· Haptic feedback devices
These simulate tactile sensations like pressure, vibration,
or resistance. Haptic gloves or instrument handles can recreate the feeling of
cutting tissue, inserting needles, or stitching skin. Example: HaptiTouch or
ImmersiveTouch provide physical feedback during simulated surgery.
1.3.1.3 Modalities of use in medical
education
VR is transforming multiple facets of medical education,
providing experiential learning in a controlled, repeatable, and safe
environment. Below are key application areas:
· Skills training: VR allows repeated practice of
clinical techniques such as incision making, endoscopy, cardiopulmonary
resuscitation (CPR) or suturing without using real patients or cadavers.
·
Chapter 1. State of Art 1.4. VR applications in cardiology
Surgical simulation: Step-by-step rehearsal of complex procedures
like laparoscopy, arthroscopy, or spinal fusion. Users receive feedback on
precision, speed, and safety.It's used by residents to supplement operating
room training.
· Anatomy education: 3D exploration of body systems with
the ability to rotate, dissect, or zoom into structures in ways that static
atlases cannot offer.
· Clinical decision-making: Virtual patients with
diverse symptoms can be examined, diagnosed, and treated in real-time. This
helps students practice diagnostic reasoning, triage, and treatment
planning.
· Empathy and communication training: Some VR
experiences place learners in the shoes of patients such as those with
dementia, vision loss, or chronic pain to foster empathy and improve
communication.
· Patient education: VR is also used to help patients
understand their upcoming procedures, reducing anxiety and improving
compliance.
· Case study: Stanford's Immersive Learning Initiative
integrated VR surgical training into its curriculum and reported that learners
demonstrated: [31]
- Increased procedural confidence
- Improved knowledge retention
- More accurate performance under pressure
1.3.2 Pedagogical benefits and cognitive impacts of
immersive technologies
Immersive technologies, especially VR, enhance medical
education by transforming how learners acquire, retain, and apply knowledge.
This section highlights their contributions through both pedagogical frameworks
and insights from cognitive science, offering controlled, responsive, and
adaptive environments for high-stakes learning.
These technologies enhance engagement and active learning in
line with constructivist learning the-ory[3], improve
retention and knowledge transfer [32], reduce cognitive load while fostering
spatial understanding [33], enable learners to receive immediate feedback and
learn from errors, support social and clinical reasoning through emotional and
empathy training [34], and strengthen self-efficacy and confidence before real
clinical practice [35], among other benefits.
1.4 VR applications in cardiology
1.4.1 Existing projects and tools in cardiology
training
The use of virtual reality in cardiology has gained momentum
in recent years, offering new ways to teach, simulate, and understand complex
cardiac procedures. Several VR-based tools and initiatives are already being
used or developed for training medical professionals in cardiovascular
medicine. Let's talk about some of these immersive solutions.
· Chapter 1. State of Art 1.4. VR applications in
cardiology
14
VCSim3 (Virtual Catheter Simulator)
VCSim3 is a virtual reality simulator designed for
cardiovascular interventions, focusing on the manipulation of catheters and
guidewires. Developed at Erasmus MC, it uses an inextensible Cosserat rod model
to simulate the mechanical behavior of these tools with sub-millimetre
accuracy. This allows trainee cardiologists to practice procedures like stent
deployment and angioplasty in a safe, virtual environment. VCSim3 enhances
surgical training by providing a risk-free alternative to traditional methods,
eliminating ethical concerns and reducing costs associated with patient,
animal, or cadaver use. Although still a prototype, it shows promising
potential for medical training programs.
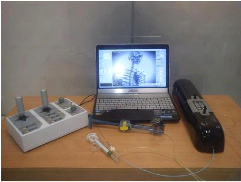
Figure 1.5: VCSim3 complete set-up including the simulator
software running on the laptop, VSP haptic device, fluoroscopic view console,
balloon inflation device, and contrast injection syringe
· VR-ECC Simulator (Extracorporeal Circulation
Training)
The VR-ECC Simulator is an advanced virtual reality training
tool designed specifically for perfusionists. It focuses on enhancing the
skills required for extracorporeal circulation (ECC), a critical procedure used
during cardiac surgeries to temporarily support the heart and lung functions.
Developed with cutting-edge technology, including Unreal Engine 4 and Autodesk
Maya, this simulator offers an immersive and interactive experience. It allows
healthcare professionals to practice and refine their techniques in a safe,
controlled virtual environment. The VR-ECC Simulator has been validated for its
effectiveness and ease of use, making it an invaluable resource for both novice
and experienced perfusionists in the medical field. [36]
Chapter 1. State of Art 1.4. VR applications in cardiology
15
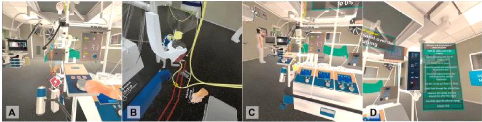
Figure 1.6: Screen captures from the virtual
reality-extracorporeal circulation (VR-ECC) simulator, featuring from
left-to-right: adjustment of the venous occluder (A), removal of the a clamp
from the arterial line (B), an overview of the heart-lung machine (C), and the
menu system by which users navigate through the simulation (D).
· vCathLab
vCathLab is an advanced medical simulation platform that uses
Virtual Reality (VR) to provide immersive and interactive training for
healthcare professionals, particularly in the field of interventional
cardiology. It allows users to practice cardiac catheterization procedures in a
realistic virtual environment, thereby enhancing their skills without the risks
associated with real procedures on patients. The platform includes authoring
tools to generate customized virtual patients and various clinical scenarios,
facilitating comprehensive and adaptable training. [37]
Figure 1.7: home page of the official vCathlab website
· Osso VR - Cardiology Modules
(with ACC collaboration)
Osso VR partnered with the American College of Cardiology
(ACC) to develop immersive left atrial appendage occlusion (LAAO) training
modules. Trainees don a VR headset (such as Meta Quest or Oculus Rift) and
rehearse step-by-step procedural workflows, including imaging control, device
manipulation, and live anatomy visualization, all within a repeatable virtual
environment. [38]
Osso VR offers trial access for educators and learners; contact
through their official site.

Chapter 1. State of Art 1.4. VR applications in cardiology
16
Figure 1.8: Image courtesy of Osso VR.
1.4.2 Comparative analysis of existing solutions and
benefits of our solution.



